Disc Herniation
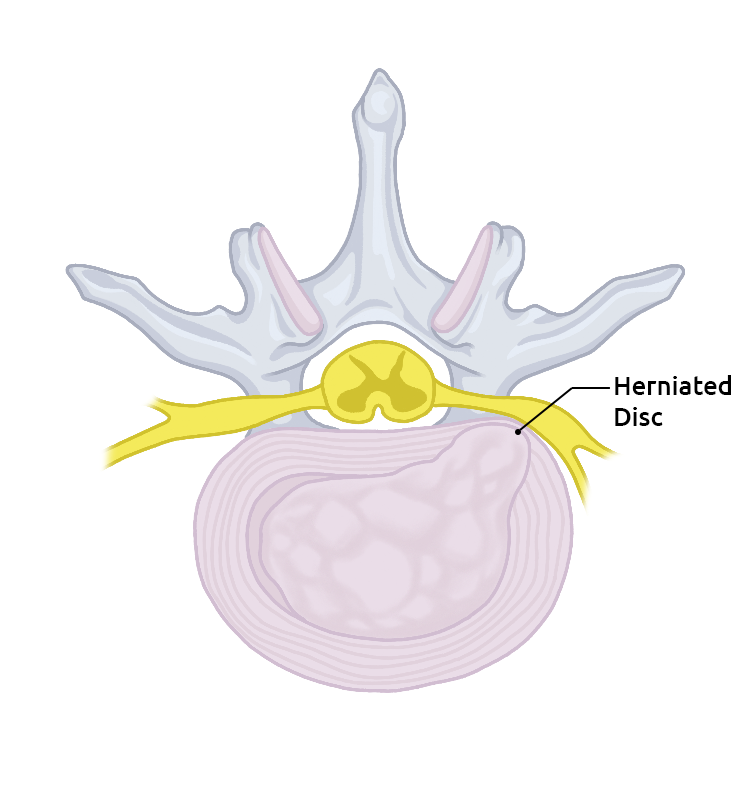
A herniated disc occurs when the nucleus pulposus, which is the gel-like inner substance of an intervertebral disc, breaks through the annulus fibrosus, which is the tough, outer rim of the tire-like structure. Pain is the most common symptom. However, nerve compression and inflammation can cause other symptoms including numbness, tingling and/or weakness in the extremities can also occur with a herniated disc.
A herniated disc can cause other symptoms, including reflex dysfunction or an abnormal reflex response in the arms or legs, depending on where in the vertebral column the disc rupture occurs.
- Cervical Spine: If a herniated disc occurs in the upper spine area, neck pain may result which radiates into the shoulders or arms.
- Thoracic Spine: Mid-spine disc herniation is uncommon. If a herniated disc occurs in this area, pain may radiate to the front or back of the body’s trunk
- Lumbar Spine: A herniated disc in the lower spine typically causes pain that may radiate or shoot into the buttocks, thighs, and legs. This is sometimes called sciatica.
Reasons
Anatomy. To better understand what happens when a herniated disc occurs, it's helpful to know a little about the anatomy of the vertebrae themselves and the different parts of the body that make up the spinal column.
In between each of your vertebrae is a cushion that acts like a shock-absorber. These are called intervertebral discs. They are sometimes compared to jelly doughnuts. Each disc has a tough outer ring made up of fibers, that is really a strong ligament that binds the vertebra together. This outer rim is called the annulus, and it is the strongest part of the disc. The center of each disc, called the nucleus pulposus, is filled with a gel-like substance. This soft center is what gives the discs their ability to act as shock-absorbers .
When a herniated disc occurs, the tough outer rim is damaged and the soft gel center moves out of its normal space. If the rim is damaged near the spinal canal, the gel material can bulge out and press into the spinal nerves or the spinal cord.
Causes of Herniated Discs. The primary reasons herniated disc occur is due to normal wear and tear on the spine and the process of aging. As we grow older, the discs between our vertebrae are negatively affected by changes that cause them to dry out and lose some of their elasticity. This is usually a slow process and the herniated disc develops gradually. Occasionally, events occur that cause a herniated disc to happen suddenly. Examples of these types of events are trauma, such as falls or other injuries such as car accidents. Lifting or twisting are other examples of events that can cause sudden herniated disc.
Most cases of true herniated discs occur in middle-aged and young adults. Children can develop herniated discs, but this occurs rarely. In the elderly, degenerative changes in the spine that normally occur with age make it less likely for a true herniated disc to develop.
If too much pressure is suddenly placed on a disc, a herniated disc can occur. One example of this can be falling from a tree and landing on the buttocks. This type of fall causes a significant amount of force to be placed on the spine all at once. If enough force is experienced, either a vertebra can break or fracture, or a herniated disc can result. Bending from the waist also places extreme force on the intervertebral discs. If you try to lift a heavy object while bending, the combination of these forces can cause a herniated disc.
A small amount of force can also cause a herniated disc. When this occurs, it is usually due to weakening in the fibrous rim of the disc (the annulus) from a repeated trauma that has added up over time. As the annulus becomes weaker, eventually too much force or pressure is applied and it herniates due to its weakened condition. You may be lifting or bending in a way that has never caused a problem before, but due to the aging process of the spine, a herniated disc occurs buy inflatable pub.
Herniated discs cause problems for two reasons. First, the gel-like substance that leaks into the spinal canal from the nucleus pulposus can exert pressure on the spinal nerves. There is also a possibility that this gel-like material released by the herniated disc causes a chemical irritation of the nerve roots. The pressure, combined with the irritation, can cause the nerve roots to not function correctly. The result of the herniated disc is a pain, and/or numbness and weakness in the portion of the body served by the affected nerve.
Prevalence
Pain in the lower back can develop for many different reasons. People use the terms "slipped disc" and "ruptured disc" very frequently and it's often assumed that every person who has pain in their back has a ruptured or herniated disc. The truth is, a true herniated nucleus pulposus, which is the medical term for a ruptured disc, is not a very common medical problem. In fact, most disorders that cause back pain are due to something other than a herniated disc.
In general practice clinics, the overall incidence of true herniated nucleus pulposus in patients who seek medical care due to new symptoms of lower back pain is less than 2%.
You may also be interested in:
What is Herniated Disk Treatment and surgery?
Herniated Disc Pain Relief to Focus on Maintaining Good Posture

Herniated disc symptoms rely on the precise level of the spine where the disc herniation happens and regardless of whether the nerve tissue is being aggravated or not. It's possible that there are no herniated disc symptoms. Be that as it may, disc herniation can cause extreme torment at the level of the spine influenced.
In the event that the disc herniation is sufficiently vast, the disc tissue can push on the contiguous spinal nerves that leave the spine at the level of the disc herniation. This can cause shooting pain in the dispersion of that nerve and as a rule, happens on one side of the body and is alluded to as sciatica. For instance, a disc herniation at the level between the fourth and fifth lumbar vertebrae of the low back can cause a shooting pain down the butt cheek into the back of the thigh and down the leg. Now and again this is related to numbness, muscle weakness, and shivering in the leg. The agony is frequently exacerbated after standing and abates with rest. This is frequently alluded to as a "squeezed nerve."
In the event that the disc herniation happens in the cervical spine, the pain may shoot down one arm and cause a stiff neck or muscle tensions in the neck. If the disc herniation is severe, it can push on spinal nerves on the two sides of the body. This can bring about serious pain down one, or both lower limbs. There can be muscle spasms on the lower points of the body and even affect the stomach and bladder. This symptom is known as Cauda Equina disorder.
Some people with a herniated disc do not experience any pain. The herniated disc symptoms come from the pressure that is placed on the spinal nerves and from irritation. Many people who have herniated discs do have pain due to other problems with their back that were present when the disc ruptured. Typical herniated disc symptoms in the lumbar area of the spine include:
- - Pain that radiates into one leg or into both legs
- - Tingling or numbness in areas of one leg or both legs is a herniated disc symptom
- - Weakness in certain muscles of one leg or both legs
- - The absence of reflexes in one leg or both legs can be a herniated disc symptom
The location of these symptoms varies depending on which nerve or nerves have been compressed in the spinal column as a result of the pain. The location of the symptoms will help your physician determine the correct diagnosis. By knowing where you are experiencing pain, your doctor will have a better idea of the location of the ruptured disc.
Diagnostic Procedures
If your physician suspects a herniated disc, he will obtain your medical history and complete a thorough physical examination as well as neurological tests. He will observe your spine while you are standing and while walking and may ask you to complete other movements to assess your mobility and balance. He will examine your spine for any sign of abnormality and will check your reflexes, assess sensation and look for any sign of weakness related to a possible herniated disc. He will ask about your pain and other symptoms.
Treatment for disc herniation can go from nonsurgical to surgical. The treatment normally relies upon the level of pain you're encountering and how far the disc has slipped from its original place.
Herniated disc symptoms and pain can go away by participating in activities that extend and reinforce the back and connecting muscles. A physical specialist may prescribe practices that can strengthen your back while decreasing your pain. Taking over-the-counter pain relievers and steering away from very difficult work and agonizing positions can also offer assistance.
While it might be enticing to avoid all physical movement while you're encountering the pain and inconvenience of a herniated disc, this can cause muscle spasms and joint stiffness. It would be better to stay as active as possible through exercises, for example, jogging.
In the event that your herniated disc symptoms do not react to over-the-counter drugs, your specialist may recommend stronger drugs. These include:
- - muscle relaxers to relieve muscle pain and spasms
- - narcotics to relieve pain
- - pain medications like Gabapentin or Duloxetine for the nerves
Your specialist may suggest surgery if your symptoms don't die down in a month and a half, or if your herniated disc is affecting your muscles. Your specialist may evacuate the harmed or jutting bit of the disc without expelling the whole disc. This is known as a microdiscectomy.
In more extreme cases, your specialist may replace the disc with an artificial one or remove the disc and join your vertebrae together. This technique helps keep your spinal column stable.
Your physician may recommend imaging tests to help confirm the diagnosis of a herniated disc symptom. He may order tests such as X-rays, an MRI or a CT scan.

Not every case of a herniated disc requires surgery. In fact, in most cases, herniated discs do not require surgical treatment. How a herniated disc is treated depends on the symptoms and whether they are resolving or getting more serious. Your doctor is more likely to recommend surgery if your symptoms of a herniated disc are steadily becoming more severe. If your condition is improving, he may recommend a course of treatment that involves watching and waiting to see if your symptoms resolve. Many patients who experience problems because of a herniated disc when it first occurs, find their symptoms completely go away over a period of several weeks or a few months.
Conservative Treatment
If there are no signs of serious complications resulting from a herniated disc, many times doctors will recommend conservative treatment of your symptoms. Conservative treatment includes:
Observation: This involves watching your condition to make sure the herniated disc does not lead to other serious complications. If there are no indications of progressive weakness or numbness, and your pain is manageable, your physician may suggest watching and waiting.
Rest: If the herniated disc causes more significant pain, your activity may need to be decreased, and you may need a few days away from your job. After resting for several days, slowly start to increase your activity with gentle tasks such as walking, and gradually increase your activity tolerance to see if your symptoms of herniated disc worsen.
Pain medications: Depending on how severe your pain related to your herniated disc is, different analgesics (pain medications) can be used to help you be more comfortable. Nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, ibuprofen, and naproxen can be purchased over-the-counter and help to decrease the inflammation and serve as a herniated disc pain relief. These drugs can cause stomach irritation, so should be taken with food. If these medications are not effective, your physician may prescribe a stronger medication to be your herniated disc pain relief such as narcotics, muscle relaxants or other types of medications. Narcotic analgesics can become addictive, and many doctors will not prescribe these for more than a few weeks for herniated disc pain relief.
Epidural Steroid Injection (ESI): An injection of a steroid medication such as prednisone directly into the affected herniated disc area to decrease the pain and inflammation is usually only suggested in cases of severe pain, or if surgery is quickly becoming the only other available treatment option. ESI is only effective as a pain control intervention about 50% of the time for herniated discs pain relief.
Surgical Treatment
Laminotomy and Discectomy
The most traditional surgical procedure for treating a herniated disc is the laminotomy and discectomy.
In this operation, an incision is made in the back directly over the herniated disc. The muscle tissues under the skin are moved so the doctor can see the backbones. It may be necessary to take X-rays during the operation to make sure the correct vertebra and disc are chosen. A small incision is made in between the two vertebrae where the herniated disc is located. This incision allows the surgeon to visualize the spinal canal. A small portion of the vertebra (the lamina) usually needs to be removed to make access to the spinal canal possible.
The surgeon then finds the gel-like disc material which has ruptured from the disc and removes it from the spinal canal. This will take the pressure and irritation off of the spine. He also removes as much of the material as he can that is still inside the disc to prevent it from leaking out (herniating) again and causing another herniated disc episode.
When the doctor is finished with the procedure, the muscles are replaced into position, and the skin incision is closed with metal staples or sutures.
Microdiscectomy
This procedure is basically the same as the traditional laminotomy and discectomy for herniated disc repair; however, the incision is much smaller. This means there is less injury to the unaffected parts of your spine during the procedure and recovery may occur more rapidly.
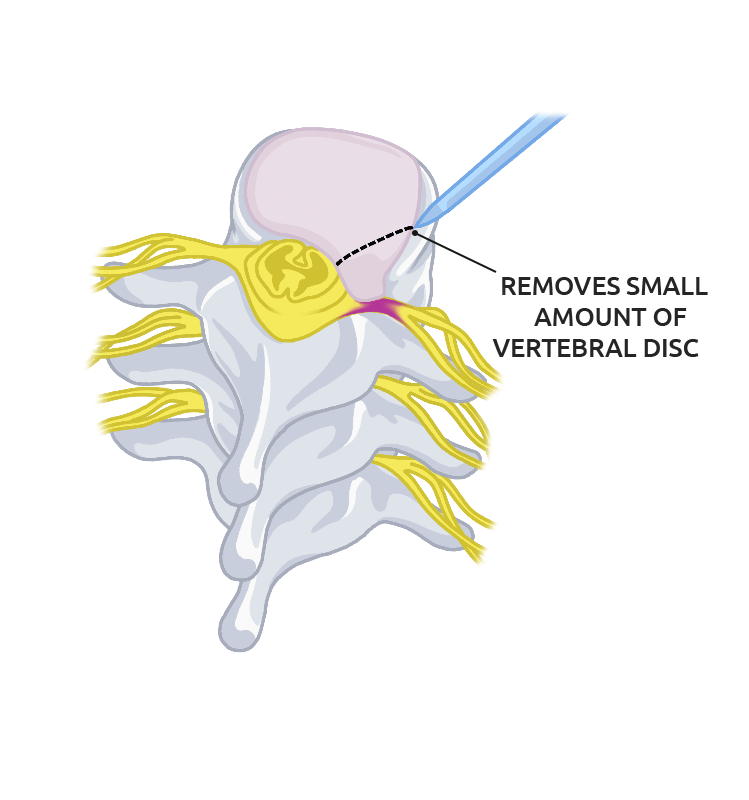
A very small incision is made just over the herniated disc, and the muscles are moved aside as in the traditional procedure. Once the herniated disc is seen, an operating microscope is inserted and used to complete the operation. The remainder of the herniated disc procedure is completed using the same approach as the traditional method.
Endoscopic Discectomy
In this herniated disc operation, even smaller incisions are needed to insert special television cameras into the spinal canal so the surgeon can visualize the herniated disc material. Other special surgical instruments are also inserted through these small incisions, and the surgeon views the TV screen and guides the instruments to remove the herniated disc material.
This procedure is not yet being widely used to repair herniated discs and is still evolving. It is beneficial in that the incisions required are very small (1/4 inch), so do even less damage to tissues around the spine than the microdiscectomy. This can mean fewer complications and faster recovery times from herniated disc surgery.
Complications:
Before surgery:
Complications from a herniated disc can occur even before surgery. Cauda equina syndrome is probably the most serious complication that can occur as a result of a herniated disc. This syndrome results when a large portion of the herniated disc material ruptures into the spinal canal in the area where the nerves travel which controls bowel and bladder function. Permanent damage to these nerves can result from pressure. If this happens, you may become incontinent (lose control) of bowel and bladder function. This is a rare, but serious condition that can result from a herniated disc. If your physician suspects this is happening, he will recommend immediate surgery to get the pressure off the nerves.
During surgery
During any type of surgical procedure, there is always the risk of complication due to anesthesia. Possible complications during an operation for a herniated disc include:
Nerve injury: Removal of herniated disc material involves working near the spinal nerves. During the procedure, the nerves may be damaged or injured. If this happens, you may suffer nerve damage, causing permanent weakness, numbness or pain in the area the nerve travels.
Dural Tear: The spinal cord and the spinal nerves are covered with a water-tight bag of tissue which is called the dura mater. During herniated disc surgery, a tear can occur in this covering and it is not unusual for this to occur in any type of operation on the spine. If the tear is noticed during the herniated disc operation, it is repaired and usually heals without further complication. If it goes unnoticed during herniated disc surgery, the tear may not heal and it can leak spinal fluid. Leakage of spinal fluid can result in problems such as spinal headaches and the risk of infection in the spinal fluid, called spinal meningitis. If the leak does not heal and seal itself on its own fairly soon after herniated disc surgery, the tear in the dura may have to be surgically repaired. This would require a second operation.
After surgery:
Some complications do not become apparent until after herniated disc surgery. Some become evident soon after your operation and others may take months to show up. Post-surgical complications following herniated disc procedures include:
Infection: All surgical procedures carry some risk for infection and herniated disc surgery on the spine is no different. Infection can develop around the nerves in the spinal canal, inside the affected herniated disc or in the incision made in the skin. If the infection involves only the incision in your skin, the only treatment needed may be antibiotics. If the infection develops in the herniated disc area or in the spinal canal, you may need further surgery to drain the infection in addition to antibiotics.
Re-herniation: There is about a 10-15% chance that the herniated disc that was operated on will herniate again. This usually occurs within the first six weeks following your surgery, but it may happen anytime. If this occurs, you may need another herniated disc operation.
Persistent pain: Herniated disc surgery does not always eliminate pain. There are many reasons people continue to have pain despite back surgery. These reasons include:
- If the nerves have been damaged by pressure caused by the herniated disc, complete recovery may not be possible.
- Scar tissue may form around the nerves following herniated disc pain relief surgery. This puts pressure on the nerves and causes pain similar to the pain caused by the herniated disc.
- The herniated disc pain you were having prior to surgery may be from issues in addition to disc herniation that was not solved by removing the herniated disc.
Degenerative Disc Disease: Any time a disc is injured, the injury can lead to degeneration in that portion of the spine. A herniated disc that has been surgically altered can certainly be considered as "injured." This places the surrounding area of the spine at increased risk for degenerative changes to occur. The degenerative process is very slow, usually taking several years to occur, but if the changes caused by degeneration become severe, a second surgery may be needed.
Rehabilitation
Following your herniated disc pain relief operation, your physician will probably recommend physical therapy before you begin an exercise routine on your own. A skilled therapist will help you choose exercises that are safe and effective for you as an individual. Exercise is essential to your herniated disc pain relief, as well as to maintain your spine health over time. It's the easiest and most sensible way to combat problems with your back.
Research has shown that exercise, done on a regular basis is linked to fewer back problems. It has many benefits for your spine health including:
- - Strengthening: It can help re-strengthen your core muscles that help support your spine following herniated disc pain relief surgery, and also can strengthen the muscles of your arms and legs. Strength in your muscles reduces back strain.
- - Exercise can reduce your risk of falling and sustaining injuries.
- - Stretching exercises decrease the risk of painful spasms in the muscles.
- - Weight-bearing exercise helps to prevent osteoporosis, which in turn decreases your risk of compression fractures that can cause pain similar to that of a herniated disc.
- - Aerobic exercise, the kind that increases your heart rate, can help to relieve pain. It stimulates the body to release its own "feel good" chemicals, called endorphins.






