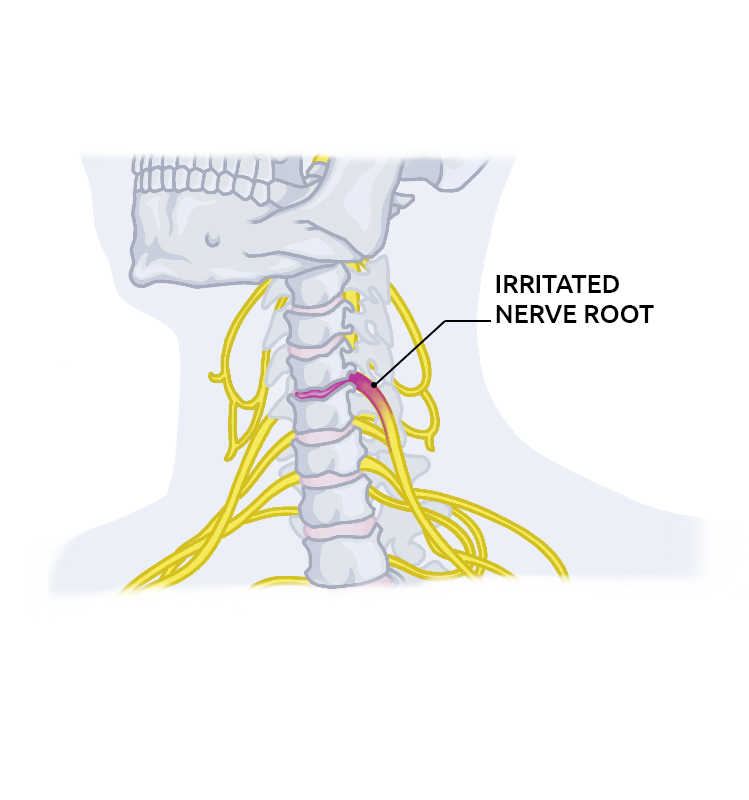
Cervical Radiculopathy

What is cervical radiculopathy? It is a condition that affects the nerve roots of the cervical or upper portion of the spine. The nerve roots that are usually affected are those of the sixth and the seventh cervical vertebrae. Damaged nerve roots can lead to pain or loss of feeling in the areas where the nerve passes through and the feeling can move to the hand. However, these effects depend on the location of the damaged root.
Types of cervical radiculopathy
When trying to understand what is cervical radiculopathy, symptoms of the condition usually differ, and this entirely depends on the affected nerve. For instance, C5 radiculopathy can happen if the nerve root running above the C5 vertebra is affected.
Even though the specific symptoms vary depending on the patient, the following are some descriptions of the types of cervical radiculopathy depending on their symptoms.
-
- C5 radiculopathy – it causes weakness and pain in the upper arms and shoulders of the patient. C5 radiculopathy can also cause discomfort around the shoulder blade area. In rare cases, this condition can bring about numbness or tingling.
-
- C6 radiculopathy – this condition mostly causes pain and weakness in the entire arm, especially in the wrists, the index finger and thumb, and biceps.
-
- C7 radiculopathy – patients with this condition usually complain about pain or weakness which can extend from the neck to the arm, especially in the triceps and the middle finger.
-
- C8 radiculopathy – it causes pain which extends from the neck of the patient to their hand. Patients normally complain about weakness in their hand grip and numbness and pain radiating in the inner part of their arm, and also in the ring and little fingers.
The cervical spine has seven cervical vertebrae, which are the bones which form the neck part of the body. These bones are separated by intervertebral discs, which absorb shock for the spine. Every cervical vertebra has a canal, which allows the spinal cord to travel through. Spinal nerve roots begin from the spinal cord and then extend to different parts of the arm. If the abnormal pressure is applied to where these nerves originate, everything along the nerve's path is affected.
The affected nerve cannot relay messages from the brain to the muscles, or receive the appropriate feeling from that part of the arm where this nerve travels through.
The following factors can cause pressure on the spinal nerves:
-
- - Arthritis or wear and tear or cervical discs.
- - Herniated or protruding discs as a result of disc degeneration or trauma.
- - Narrowing of the spinal canal.
- - Tumor intruding the nerve root.
Prevalence
Cervical radiculopathy does not happen nearly as often as lumbar radiculopathy, a condition that affects the lumbar or lower portions of the spine. Cervical radiculopathy affects people of all ages, and they require cervical radiculopathy treatment exercises to manage the condition.
Research has shown that the following mechanisms are responsible for causing nerve root impingement or irritation:
-
- Spondylosis – it is more common in elderly people and causes bony spurs or stenosis.
-
- Disc herniation – it is prevalent among younger people.
According to statistics, cervical disc herniation accounts for 20% to 25% of cervical radiculopathy cases in young people. Herniated discs in younger people mostly occur because of an injury that causes a pinched nerve. In older patients, the condition is usually the result of changes brought about by aging, such as degenerative changes. Bone spurs often occur as a result of normal wear and tear on the spine and its supporting structures. Intervertebral discs become dry and shrink as a result of the aging process. Doctors say that most of the aged people show symptoms of the above conditions when turning up for cervical radiculopathy treatment exercises.
This condition mostly affects people between the ages of 40 to 50 years, at a reported prevalence rate of 51.03%. A research conducted in the US regarding the prevalence of cervical radiculopathy showed that the condition is less prevalent compared to lumbar radiculopathy. Statistics from the research indicate that out of every 100,000 people, 83 of them have cervical radiculopathy.
Cervical radiculopathy occurs more frequently in women than men, as it accounts for 53.69% of all the reported cases. Close to 50% of all cervical radiculopathy patients in the US live in large metropolitans. 39.27% of cases are reported to be from southern regions in the United States. A study conducted in Minnesota revealed the rate at which common nerve root compressions occurs:
-
- - C7 at a rate of 46.3% to 69%
- - C6 at a rate of 17.6% to 19%
- - C5 at a rate of 2% to 6.6%
- - C8 at a rate of 6.2% to 10%
The incidence of neck pain as a result of cervical spondylosis which contributes to cervical radicular in adults is estimated to be between 20% and 50% every year. Statistics show that cervical spondylosis affects both men and women at the same rate. An estimated 95% of people aged 65 years and above are affected by cervical spondylosis to some level, and researchers say that it is the major contributor to spine dysfunction in aged people.
75% of people above the age of 50 have shown notable signs of a narrowing spinal canal, and 50% of these incidences are symptomatic. The number of symptomatic cases increases to 75% for people aged 65 and above. Changes in the cervical spine because of spondylosis happen at the single level of every disc space in 15% to 40% of patients and multiple levels of disc space in 60% to 85% of patients.
Risk factors
There are some known risk factors associated with the development of cervical radiculopathy. Also, some of the risk factors are cervical radiculopathy causes. They include:
-
- Smoking – Smoking affects almost every tissue and organ in our bodies, including the spine. Smoking is among the main causes of degenerative disease, which weakens the vertebral discs. The degenerative disease can lead to an individual developing cervical radiculopathy, so, smokers are at a higher risk of developing the condition.
-
- Operating vibrating equipment – vibrating equipment, especially which require us to use a lot of energy, exert some pressure on our cervical spines. Handling the equipment for a long time can make the cervical discs to burst, causing a lot of pressure to the nerves. People handling vibrating equipment are therefore at a considerable risk of cervical radiculopathy.
-
- Poor posture – poor neck posture is mostly overlooked when trying to determine cervical radiculopathy causes. What you should understand is that poor neck posture can cause an individual to have weak neck muscles. This can cause pain which extends from the neck to the arms.
-
- Poor sleeping positions – people with poor sleeping habits can strain their spines and cause damage to their cervical discs. If the discs are affected to the point where the surrounding nerves are also affected, the person can be at risk of developing cervical radiculopathy.
-
- Frequent lifting of more than 25 pounds – lifting heavy objects can put pressure on cervical discs. The prolonged exertion of pressure to these discs can make them crack or collapse, placing the person at risk of cervical radiculopathy.
-
- Age – as a person grows old, their intervertebral discs become stiff and provide less support to the spine. In addition, their bones and ligaments thicken and begin to intrude on the spinal canal, leading to a condition known as cervical spondylosis.
-
- Occupation – some jobs involve a lot of repetitive neck movements, uncomfortable neck positioning or doing overhead work, activities that strain your neck. Engaging in such activities for a prolonged period is likely to put you at risk of cervical radiculopathy.
-
- Neck injuries – people with a history of neck injuries are at an increased risk of developing cervical radiculopathy.
-
- Genetic factors – people from families with a history of cervical radiculopathy are more likely to develop the condition compared to those without any history.
-
- Engaging in high-impact or rough sports – some sports put more pressure on the neck, putting the players at a high risk of developing cervical radiculopathy.
-
- Other risk factors that are less frequently associated with cervical radiculopathy include spinal tumors, giant cell arthritis, and spinal infections.
Additionally, people with the following conditions risk developing cervical radiculopathy.
-
- -Bone spurs or osteophytes
- -Individuals with spinal stenosis
Reasons
While the symptoms of cervical radiculopathy have been extensively studied and documented, how this condition develops has still not been fully understood. The most common symptoms of cervical radiculopathy have their roots in the inflammation that results from the compression of nerve roots.
It is thought that substances are released by bulging or herniated discs causing the nerve roots to become inflamed and swollen. The pressure on the nerve roots may be caused by a breakdown in the spinal discs – a normal part of aging, changes in the vertebrae, or other factors that eventually lead to cervical radiculopathy.
Research has shown that patients with cervical disc disease experience pain similar to that of cervical radiculopathy when a nerve root is pinched or compressed. All the same, when pressure is exerted on a disc, pain is felt in the neck and along the inner edge of the shoulder blade. Additionally, there have been instances in the past where muscle spasms have been produced by electrically stimulating discs.
The main causes of cervical radiculopathy include:
Cervical herniated disc
Herniated discs mostly occur when too much pressure is applied to a healthy intervertebral disc. For example, a car accident can lead to herniated disc if your head hits the windshield. Such accidents apply too much force on the neck, a force which can’t be evenly absorbed by a healthy neck. This leads to an injury.
The different movements of our necks cause different kinds of pressure on the spinal bone and disc. The disc acts as a shock absorber to the pressure applied to the vertebrae. The disc between the vertebrae is compressed if you bend your neck forward. Consequently, this exerts a lot of pressure on the disc, causing a swelling that extends toward the spinal cord and the nerve roots.
The cervical herniated disc can also happen as a result of a disc being weakened by a degenerative process. Once the disc has been weakened, it can rupture or tear even with the tiniest pressure being applied to it.
The pressure causes the internal material of the affected cervical disc to leak out and cause inflammation to the nearby nerves. In fact, most cervical radiculopathy cases seen in young people between the ages 20 and 30 show symptoms of cervical radiculopathy related to cervical herniated disc.
Cervical degenerative disc disease
When a cervical disc degenerates, it becomes stiffer and flatter, making it susceptible to collapse because of the degenerative disease. Affected cervical spine discs usually don’t offer the required support to the spine. The body reacts to the collapsed disc by developing more bone, known as bone spurs, in order to strengthen the affected disc. These bone spurs can stiffen the spine and the small openings where the nerve roots exit on the spinal column and pinch the nerve root.
In some scenarios, cervical degenerative disc disease can cause inflammation of the nerve root near the affected disc. The inflammation causes pain which begins from the neck and runs down all the way to the hand. At times, a person can experience numbness in areas where the nerve provides feeling. Cervical degenerative disc disease is the main cause of cervical radiculopathy in individuals aged 5 years and above.
Cervical spinal stenosis
Cervical spine degenerative processes can tighten the area of the spine where the nerve roots exit thus causing pressure to the nerves. Cervical spinal stenosis causes cervical radiculopathy related symptoms in people aged 60 and above.
The following are the typical cervical radiculopathy symptoms:
-
- - Pain that starts in the upper-mid back and spreads into the shoulders, extending down into the arms, or into the chest and neck
-
- - Weakness in the muscles and tingling feelings or loss of feeling in the hands or fingers
-
- - Decreased coordination in the fingers and hands can also be a symptom of cervical radiculopathy
The symptoms of the condition vary, depending on which nerves are affected.
Cervical radiculopathy that affects the nerve near the C5 vertebra will typically cause weakness and pain in the upper arms and shoulders, especially in and around the shoulder blades.
Radiculopathy affecting this portion of the spine rarely results in a pins-and-needles feeling, which is mostly accompanied by numbness or tingling.
One of the most common locations where cervical radiculopathy occurs is near the C6 vertebra. This causes weakness and/or pain in the entire upper extremity, from the front upper arm muscles (the biceps) all the way to the index finger and thumb.
The most common type of cervical radiculopathy is C7 radiculopathy. This causes weakness and/or pain extending from the neck down into the hand. It may include the muscles in the back of the upper arm (the triceps) and the middle finger of the hand.
C8 radiculopathy may cause a weak hand grip as well as cervical radiculopathy pain and numbness or weakness extending from the neck down to the hand, radiating along the inside surface of the arm, ring finger and little finger. These effects can affect the patient’s ability to hold or lift things, as well as their ability to perform daily tasks like getting dressed or writing.
Compression of a nerve root can cause the following reactions:
-
- - Inflammation of the affected nerve
- - Changes in vascular reaction
- - Intra-neural oedema
The above factors are the leading causes of cervical radiculopathy pain. It is also good to understand that nerve root compression should not be overlooked. The patient should take steps to deal with it even if he or she does not experience radiating pain. The same applies to the motor and sensory dysfunction, which might have an effect on you without any notable pain.
In the majority of cases, cervical radiculopathy symptoms are experienced when the neck is flexed towards the area radiating pain and also when inflammation happens as a result of movements of the neck. The condition will typically reduce the range of motion of the cervical spine, eventually causing a stiff neck.
These symptoms, in turn, lead to minor musculoskeletal problems which are marked by weakness, stiff joints, postural defects, capsule tightness and the decrease in the length of cervical spine muscles. The problems can then affect the movement mechanisms of the patient’s body. Elderly people may complain about experiencing sporadic episodes of pain around the neck area or they may have some history of cervical spine arthritis.
Diagnostic procedures
Before treating any symptoms related to cervical radiculopathy, a doctor will have to make a cervical radiculopathy diagnosis in order to understand the factors causing the symptoms. For instance, both carpal tunnel syndrome and cervical radiculopathy share some symptoms like numbness and pain in the hand. So, differentiating the two conditions is paramount if the patient is to receive the right treatment.
Almost always, the doctor will ask about your medical background and if you have any history of certain illnesses, accidents or injuries. He will also want to know your family’s medical history. Depending on these conditions plus your lifestyle, the doctor will most probably have a good understanding of what needs to be investigated further.
If your doctor suspects you have cervical radiculopathy, he will likely recommend several tests to identify the actual cause of the condition. Tests may include:
-
- X-rays: Bone alignment and narrowing of the disc spaces can be identified on x-ray. X-rays can also show if the foramen has narrowed and if there is any damage to the discs.
-
- MRI: This test uses magnetic resonance imaging to look at the spinal cord, the nerve roots and the soft tissues surrounding the spinal cord. MRI scans on your neck can help the doctor determine if there are nerve compressions caused by damaged soft tissues – like herniated or protruding disc. The scan can also assist the doctor towards understanding whether your spinal cord or nerve roots are damaged.
-
- CT scan: This uses computerized tomography to examine the minute details of the bones and possible bone spurs that may be causing cervical radiculopathy.
-
- EMG: An electromyogram is used to measure the electrical activity of the muscles at rest and during contraction and can determine if there is nerve damage. Also, nerve conduction tests are performed alongside EMG to check if the nerves are okay. Both of these tests can assist your physician to know whether your symptoms are as a result of nerve damage, pressure on your spinal nerve roots or other conditions which cause damage to your nerves, like diabetes.
-
- NCS: This is a nerve conduction study. It tests the ability of the nerves to send electrical impulses.
Other tests include:
Physical exam – in this examination, the doctor feels the patient’s neck for tenderness or any abnormalities, and the neck’s range motion and strength.
Spurling’s test – this test is often part of the physical examination. During this cervical radiculopathy diagnosis, the doctor checks to see if compressions to the cervical spine lead to the symptoms or worsen the radicular symptoms the patient is experiencing. Generally, this test requires that the patient bends their head to show the area where they are experiencing symptoms of cervical radiculopathy.
The doctor then applies pressure very gently on top of the patient's head. This process is very effective as it replicates the symptoms of cervical radiculopathy. If the test replicates the cervical radiculopathy symptoms the patient is complaining about, then it is likely that the patient has cervical radiculopathy.
Spurling’s test is recommended for patients showing cervical radiculopathy as a result of a traumatic injury which might have caused a fracture in their spine.
Did you know that most cervical radiculopathy symptoms don’t require any treatment? In fact, some of these symptoms disappear with little or no intervention of any kind. However, if an individual doesn’t show any improvement, they should consider undergoing treatment for cervical radiculopathy. The treatment can either be conservative or surgical depending on the nature and severity of the condition.
Conservative Treatment
Conservative cervical radiculopathy treatment is usually the first step in treating the condition.
-
- Medication: Certain medications can be very effective to treat the pain and inflammation caused by a compressed nerve:
-
- - Analgesics
-
- - Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, aspirin, and naproxen
-
- - Muscle relaxants
-
- - Oral corticosteroids
-
- - Narcotic analgesics are sometimes used to treat severe pain caused by cervical radiculopathy
-
- - Injections of steroids into the affected area
-
- Physical Therapy: Exercise can be used to help relieve the pain caused by cervical radiculopathy. Typically, a skilled therapist will use modalities such as ultrasound, heat or ice to help reduce pain and muscle spasms. Physical therapists can also work with patients and their physicians to find adaptive equipment and braces such as cervical collars to help provide support and rest for the cervical spine.
- Medication: Certain medications can be very effective to treat the pain and inflammation caused by a compressed nerve:
-
- Cervical traction: In some cases, traction can help decrease the pressure on the nerve root. This doesn’t help in all cases of cervical radiculopathy, but it’s simple to do and in cases where it is effective, the patient can use a home traction device to obtain relief.

-
- Activity modification: Some activities make pain worse and need to be avoided lest they irritate the nerve root. Activities to be avoided may include heavy lifting (over 25 pounds), any activity that causes vibration and compression of the cervical spine, such as boating, running, jogging and snowmobile riding, and any activity that requires prolonged neck extension or rotation.
Surgical Treatment for Cervical Radiculopathy
If the pain from cervical radiculopathy persists longer than 6 to 12 weeks, or if it causes severe disability, spinal surgery may be recommended. Surgery for a herniated cervical disc usually carries little risk of complications. It can be completed in a number of different ways:
-
- Cervical laminectomy – this surgical procedure is done to relieve the pressure applied to the spinal cord or the nerves surrounding the cervical region. During this surgery, the surgeon makes an incision in the lower back and then removes the tissue responsible for causing pressure on the nerves. Once the tissue has been removed, more space is created in the spinal canal, thus relieving the pressure on the cervical bones.
-
- Cervical laminoplasty – cervical laminoplasty relieves the pressure exerted on the nerves located in the neck. A surgeon makes an incision in the midsection of the neck and then manipulates the tissue that causes pressure on the nerves. The main purpose of this procedure is to widen the spinal canal.
-
- Micro cervical discectomy (MCD) – this is a surgical procedure for treating people affected by cervical disc herniation. During this minimally invasive procedure, the surgeon uses a specialized surgical tool with a microscope attached to its tip to get a view of the affected area. The affected disc is removed, relieving the pressure on the nerves or the spinal cord.
-
- Cervical foraminotomy – this is another surgical procedure also performed to relieve pressure on the affected nerves or the spinal cord. The surgeon makes an incision on the back of the neck, often near the affected nerves, and then separates the soft tissues to widen the opening where the affected nerves exit the spine. Consequently, the pressure on the spinal cord or nerves is removed. The surgery is also performed to boost the stability of the spin by removing collapsed discs.
-
- Anterior cervical discectomy and spine fusion: This is the most common surgical procedure for cervical herniated discs that may be causing cervical radiculopathy. The affected disc is extracted through the front portion of the neck, a bone graft is placed and space is fused. A plate can be placed in front of the fused portion to add stability and to help ensure fusion.
-
- Anterior discectomy without spine fusion: In this procedure, the affected disc is removed through the front of the neck, but space is left open without fusing. Space will often fuse on its own but healing sometimes takes longer and often heals in a deformed position.
-
- Posterior cervical discectomy: This procedure is more difficult to perform than the anterior approach because the surgeon has to manipulate the spinal cord to get to the affected disc to correct the cervical radiculopathy.
Surgical Risks
Although serious complications from cervical disc surgery to correct cervical radiculopathy are rare, any major surgery carries the risk of complications. Possible complications from surgery for a herniated cervical disc include:
-
- - Damage to the trachea or to the esophagus.
-
- - Damage to one of the major blood vessels in the neck.
-
- - Damage to the nerve to the voice box, resulting in a hoarse voice. This typically resolves in a few months.
-
- - Failed fusion or displacement of a fusion
-
- - Nerve root or spinal cord damage
-
- - Infection can be a complication of cervical radiculopathy surgery
-
- - Cerebrospinal fluid leakage
Post-operative care
Many surgeons require their patients to wear a neck brace following a cervical discectomy that was completed to treat cervical radiculopathy. They will also ask their patients to limit their activity for several weeks post-operatively. Neck pain following surgery is common and analgesics will be prescribed to help manage any surgical discomfort after a procedure for cervical radiculopathy.
You may also be interested in Cervical Radiculopathy Exercises