Cervical Osteochondrosis
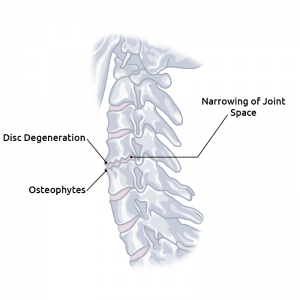
Cervical osteochondrosis is a condition that results when changes begin to occur in the cushioning discs which lie between the vertebrae in the neck. The changes in these discs cause changes in the neck vertebrae and joints themselves to also occur, resulting in compression of the nerve roots called osteochondrosis. This causes the height of the discs to be reduced and its physiological function becomes lost, resulting in the instability of the vertebral joints.
Osteochondrosis can happen in any section of the spine. This can include the cervical spine, thoracic spine, and lumbar spine. Most of the time, it's a crawling process that includes back pain which first just happens when you exert effort.
Osteochondrosis grows with age. To a specific degree, indications of degeneration in the spine are typical indications of growing old. For instance, minor serrations related with osteochondrosis occur in 90% of men who are ages 50 and above. An illness happens when immense changes result in serious issues right off the bat. This propensity is conceivably advanced by the humanized way of life. It brings about degeneration in the vertebral joints, makes wear and tear the ligament in the joints, and prompts joint inflammation. The outcome is the hardening or stiffening of the joint causing osteochondrosis.
Prevalence
Cervical osteochondrosis is a widespread condition, with approximately 80% of people worldwide suffering from osteochondrosis at some time over the course of their life. The incidence of the condition is increasing. Eventually, cervical osteochondrosis can lead to generalized osteochondrosis, meaning it affects the entire spine, or it can remain localized in one area (the cervical, thoracic or lumbar spine). When osteochondrosis remains localized in the neck, it is sometimes also known as cervical spondylosis mechanical bulls.
Our spinal discs begin to deteriorate when we are 20-years of age. The expanding loss of water prompts a decrease in the tallness between the vertebrae (chondrosis). This implies the disc is not any more ready to work as a safeguard and the strain in the front and back longitudinal tendons is lost. Therefore, over the top anxiety is put on the vertebral joints, the tendons of the spine are stacked inaccurately and the portable fragments of the spine turn out to be precarious.
Cervical osteochondrosis has developed substantially more now and can be found in young people – all thanks to the inactive way of life and mostly due to long periods of time in front of a computer. Grown-ups, for the most part, have cervical osteochondrosis mostly due from their office occupations and by driving a considerable measure – these exercises give abundance stack on the neck, intervertebral discs, and bone tissue.
Risk Factors of Osteochondrosis
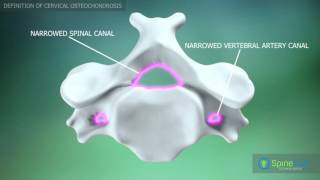
Changes in the statics of the spine happen with changes to the muscles and tendons, including the shortening of these tissues. This is joined by lost capacity and strain in the muscles (myogelosis). The ligament in the vertebral joints deteriorates sooner than regular because of the incongruent position of the joint surfaces. Also, huge insecurity causes a degenerative increment in spine ebb and flow (scolioses, kyphoses). Hypertrophic degeneration of the joint (spondylarthrosis) causes narrowing of the spinal channel (spinal waterway stenosis).
Regular variables incorporate worry, decreased blood supply to the influenced area, and as well as injury deep down. Osteochondrosis can likewise happen because of athletic movement and games wounds.
Aging is the most widely recognized reason for osteochondrosis, yet other hazard factors that improve your probability of building up osteochondrosis include having long stretches in the car, bad smoking habit, a long time of physical work, or even a past spine surgery.
Diverse eras having an inclination to cervical osteochondrosis is truly settled that the more youthful era begins having issues somewhat prior, now and then even at high school age (that was not prior), in correlation with delegates of the senior era of a family. The general population who were conceived 60-70 years prior interestingly deliver to restorative establishment concerning osteochondrosis of cervical division in developing or even at cutting edge age, and here the general population who were conceived 20-40 years back regularly as of now at youthful age have issues with a spine. It vouches for the significant decay of strength of the more youthful era associated with an idle picture in life and in work.
There are several reasons why cervical osteochondrosis may occur. They include:
-
- Genetics: If a close relative, such as a parent or sibling had or has osteochondrosis, you might be more likely to develop the disorder.
-
- Age: The older you get, the more likely you are to develop the condition. This is the most common cause of osteochondrosis.
-
- Other diseases: Having other metabolic and endocrine disorders increases your risk of developing osteochondrosis.
-
- Certain work and leisure activities: Being consistently involved in activities that place continued tension and stress on the neck muscles increases your risk of having osteochondrosis. For example, typists, drivers, lab workers, or people who watch television or play computer games for extended periods.
-
- Stress: Increased emotional stress places you at increased risk for developing cervical osteochondrosis. This helps to explain why determined and energetic individuals often are affected.
You may also be interested in Scheuermann’s Kyphosis (Osteochondrosis)

To better understand cervical osteochondrosis symptoms, it's helpful to know a little about the anatomy of the neck. One of the largest blood vessels in the body, called the vertebral artery, runs through the spinal column in the neck. This artery carries oxygen and vital nutrients to the parts of the brain that control functions such as balance, motor control, regulation of emotions, short-term memory, heart rate and blood pressure control and control of digestion and urinary function.
Cervical Osteochondrosis Symptoms
Osteochondrosis can be depicted as unmanageable back pain that's hard to handle and mostly depends on which segment of the spine. Osteochondrosis symptoms may stay constrained to the spine or emanate into the legs or arms. Osteochondrosis symptoms may be experienced either during rest, effort, or motion.
Often times, there are no cervical osteochondrosis symptoms. However, sometimes the condition results in the space that is needed by the spinal cord and the nerve roots, as well as the vertebral artery, to become too narrow. If the nerve roots, spinal cord or artery become compressed, cervical osteochondrosis symptoms might develop. Cervical osteochondrosis symptoms may include:
-
- - Pain and stiffness in the neck is a symptom of osteochondrosis
-
- - Numbness, tingling sensation or weakness in the hands, arms, feet or legs
-
- - Difficulty in walking or loss of balance and impaired coordination
-
- - Emotional changes can be a cervical osteochondrosis symptom
-
- - Ringing in the ears
-
- - Memory loss is sometimes a cervical osteochondrosis symptom
-
- - Loss of bowel or bladder control is one of the most important osteochondrosis symptoms to look out for
-
- - Decreased range of movement
-
- - Popping and locking of joints
-
- - Inability to straighten the affected limb
-
- - Poor coordination
-
- - Unstable pressure
-
- - Reduced vision and hearing
-
- - A constant sense of discomfort in the neck are
-
- - Dizziness
Diagnostic procedures
If your physician suspects cervical osteochondrosis due to osteochondrosis symptoms, he will perform a thorough physical examination. Included in the examination, he will most likely check the mobility of your neck. Your doctor will also check your reflexes and your muscle strength to find out if there is any pressure on your spinal cord or your spinal nerves caused by cervical osteochondrosis. You may also be asked to walk so the doctor can see whether spinal compression caused by cervical osteochondrosis has had any effect on your gait.
Imaging tests
Diagnosing osteochondrosis involves three steps. The first is that your specialist will start by taking your therapeutic history before directing a physical exam. In the wake of digging into your health history and playing out a physical exam, your specialist will direct some neurological tests and imaging tests to see the degree of the ligament harm. An MRI is normally the most valuable imaging test.
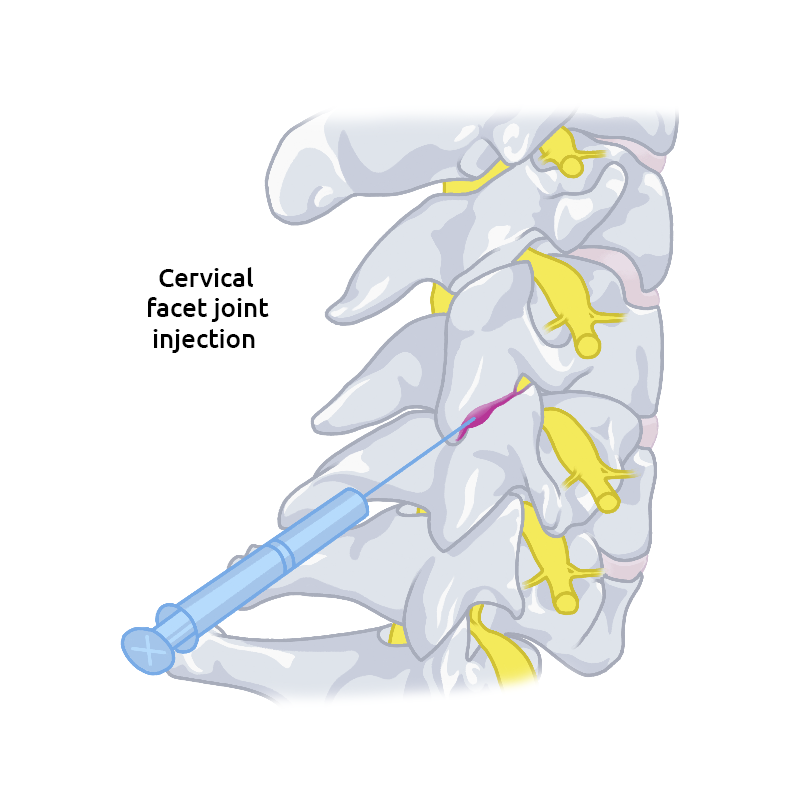
Treatment of the condition relies upon the seriousness of the disease's side effects. The objective is to balance out the spine, so exercise based recuperation is frequently one of the main preservationist treatment alternatives. Other nonoperative treatment methods include:
-
- -Over-the-counter drugs
- -Heat therapy
- -Injections
- -Motion exercises for relaxation
In order to guide your diagnosis and treatment, your physician may order special imaging tests. Tests for cervical osteochondrosis may include:
-
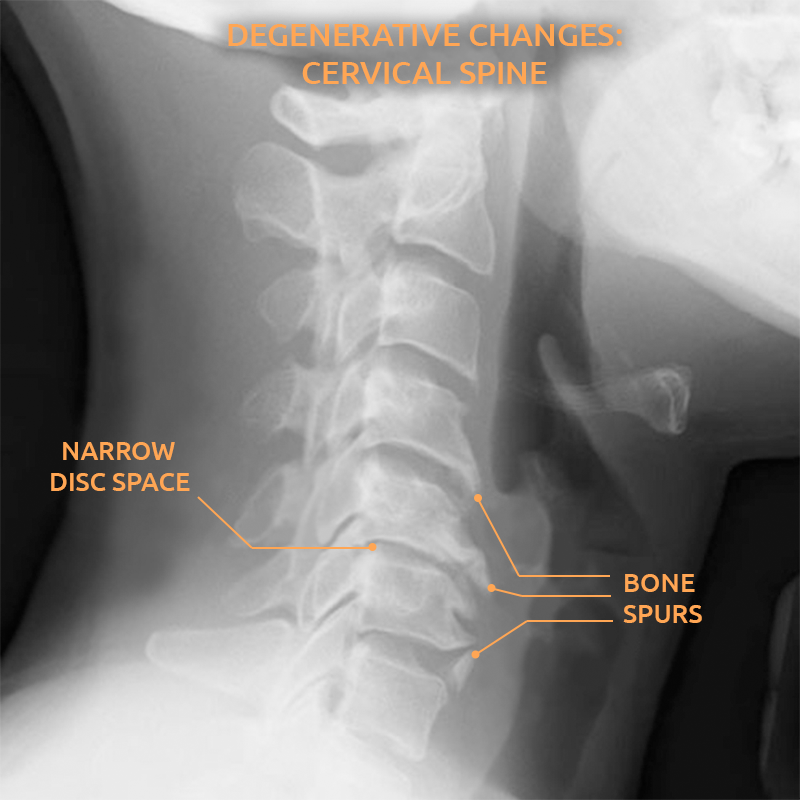
- Neck X-ray: Abnormalities may show up on an X-ray that indicates cervical osteochondrosis, such as bone spurs. Most often, X-rays are ordered as screening tools to rule out serious causes of neck stiffness and pain such as infections, fractures or tumors.
-
- Computerized tomography (CT scan): This study uses X-rays taken from several different angles and combines them to give your doctor a cross-sectional image of your neck vertebrae and other structures. A CT scan is much more detailed than a plain X-ray and provides more information, especially related to the bones and may be suggested if your doctor suspects cervical osteochondrosis.
-
- Magnetic resonance imaging (MRI): This test uses radio waves and a strong magnetic field to provide your doctor with cross-sectional views of soft tissue and bones. This can help determine areas in your neck and spine where nerves may be compressed due to cervical osteochondrosis.
-
- Myelogram: This study is used with X-rays or a CT scan following the injection of dye to make the spine more visible and assist with spinal conditions such as cervical osteochondrosis.
Nerve function tests
Nerve function studies are sometimes ordered by your physician to help find out if the signals sent by your nerves are being sent and received properly by the muscles. These studies include:
-
- Electromyogram (EMG): This study assesses how healthy your muscles and nerves are by measuring the electrical activity of the nerves when they send messages to the muscles when the muscles are at rest and when they are contracting. If your doctor suspects nerve function is impaired by cervical osteochondrosis, nerve function studies may be ordered.
- Nerve conduction study: This test measures the speed and the strength of the signals sent by the nerves. Electrodes are attached to the surface of your skin, and a small shock is administered to the nerve being studied.

Cervical Osteochondrosis Treatment
Cervical osteochondrosis treatment depends on how severe your symptoms are. The goals of treatment focus on helping to relieve pain, helping you continue the activities you normally enjoy as much as possible and preventing disabling injury to the nerves and spinal cord.
Osteochondrosis treatments can be separated into nonsurgical and surgical methods. Therapeutic and steady treatments constitute the backbone of osteochondrosis treatments. Surgery is demonstrated just for particular purposes, for example, easing of indications, or incapacity. In spite of the fact that the course of an osteochondrosis treatment is extended, it is by and large self-constrained.
Medications
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are many times very effective for controlling the pain and inflammation and serves as a cervical osteochondrosis treatment. These medications are available without a prescription, but they can cause some stomach upset so they should be taken with food.
If these medications are not effective for controlling pain as an osteochondrosis treatment, your doctor may recommend prescription medication. For example, he may suggest:
-
- Muscle relaxants: These medications are helpful in controlling painful muscle spasms associated with cervical osteochondrosis and include drugs such as methocarbamol (Robaxin) and cyclobenzaprine (Flexeril).
-
- Anti-seizure medications: Some kinds of drugs used to treat epilepsy also work well to control nerve pain, like that which occurs with cervical osteochondrosis. These include medications such as pregabalin (Lyrica) and gabapentin (Neurontin).
-
- Narcotics: In some cases of severe pain, physicians will order analgesics that contain narcotics. Examples of these are oxycodone (Percocet) or hydrocodone (Vicodin).
-
- Steroid injections: Injecting a steroid such as prednisone, along with an anesthetic, directly into the affected area is recommended in some cases of cervical osteochondrosis.
Therapy
Physical therapy is recommended in some instances of cervical osteochondrosis treatments. A trained therapist can instruct you in exercises that will strengthen and stretch the muscles in your shoulders and neck. Traction is sometimes beneficial as it can help make more room within the spinal column and relieve the pressure on the nerve roots which are being pinched in some patients with cervical osteochondrosis.
Surgery
Surgical osteochondrosis treatment is generally attempted when preservationist strategies are ineffectual or coming up short or when they are relied upon to fall flat on development. Another sign for surgical treatment is a circumstance where such treatment may help re-establish the reparative procedure or guide this procedure so as to enhance results. What's more, surgery is some of the time performed to upgrade the patient's corrective appearance.
Although full recuperation after surgery is remarkable, it has been known to happen even in cutting-edge cases, given the proper setting. In this manner, surgery is best conceded until late over the span of the sickness, or else held for the treatment of handicap.
If your condition is getting worse, cervical osteochondrosis may cause you to begin to develop weakness in your extremities. If this occurs or if your signs and symptoms are not any better despite conservative treatment, your doctor may recommend surgery to create more space for your spinal cord and nerve roots. Sometimes this requires the removal of bone spurs or a herniated disc, or it could involve the removal of a portion of a vertebra as the osteochondrosis treatment.
Pathological changes
Cervical osteochondrosis causes changes which have an effect on the vertebrae, the intervertebral discs, and the surrounding tissues. The vertebrae in the neck are not as stable as those in other parts of the spine, and they can easily become displaced. When this happens, the canal that the vertebral artery travels through can become narrowed, causing a lack of blood and oxygen supply to the areas of the brain it supplies. The canal the nerves pass through, from the spine to the brain can also narrow. This may cause symptoms, such as those of cervical osteochondrosis, to occur in the neck and the upper extremities and possibly cardiac and respiratory symptoms, as these nerves also influence these functions.
Follow-up is required after surgery to elevate mending and to keep up the outcomes accomplished. Ensured preparation took after by useful action is fundamental whether the osteochondrosis is dealt with conservatively or surgically at any stage. Follow-up is long, expanding numerous years to the point that skeletal development is accomplished. Since the infection may erupt or exacerbate, an alternate method might be required sooner or later.
On the off chance that the life systems and physiology of the joint are reestablished after skeletal development, the danger of industrious dreariness is low. Be that as it may, poor reclamation is basic on account of auxiliary osteoarthritis and related inability. In the event that these sequelae emerge, fitting intercession is important.
A guided physiotherapy program must be at the same time embraced amid restoration with the point of diminishing incapacity.
You may also be interested in Scheuermann’s Kyphosis (Osteochondrosis)