Compression fractures of the Spine

Compression fractures of the spine are breaks that occur in the vertebrae under the force of pressure. Your vertebrae are the bones that make up your spine. The spinal fracture is often defined based on its location along the spine. These breaks most commonly happen in the middle (thoracic) and lower (lumbar) areas of the spine.
A spinal fracture happens when the vertebrae become pressed together because of trauma. In most situations, the amount of force necessary to break a spinal vertebra is substantial, but in some situations, such as in people who have cancer, or in the elderly, the vertebrae become fragile and spinal fractures can occur with very little force. While it most often occurs in the lower back area, it can happen in any area of the spine.
Multiple compression spinal fractures are a result of fractures affecting more than one vertebra. These spinal fractures lead to a forward rounding of a person’s spine, thus making them look shorter or causing kyphosis. Elderly people are the main victims of spinal fractures, although the prevalence is very high among women.
The pain caused by a compression fracture of the spine varies depending on the patient and the location of the spinal fracture. Some people complain about experiencing severe pain, while others don’t show any signs of pain at all. Severe spinal fractures of the spine can lead to a forward curvature of the spine, a condition is known as kyphosis or dowagers hump.
Osteoporosis is the common cause of compression fractures of the spine and it leads to the following types of spinal fractures:
-
- Wedged fracture – the compression fracture happens in the anterior of the vertebra and it causes the bone in front of your spine to collapse, but this doesn’t change the back of the same bone. As a result, a wedge-shaped vertebra is formed.
-
- Crush fracture – spinal fractures happen in cases where the whole bone breaks.
- Burst fracture – people with this type of fracture are known to lose some height in both the posterior and anterior walls of their vertebral body making this crush fracture very distinct as height loss from other spinal fractures happen in the anterior of the vertebra. Thus, it is very important to make this distinction, as burst spinal fractures can lead to neurologic compromise or progressive deformity.
These three spinal fractures can also be classified as either stable or unstable.
-
- Stable fractures are unlikely to undergo any further changes and therefore there is little possibility of the spinal fractures creating additional damage.
-
- Unstable fractures are more likely to undergo further changes. These changes can cause damage to the tissues and nerves, or lead to permanent spinal deformity.
Causes of Spinal Fractures
Compression fracture of the spine can be caused by various conditions including trauma, osteoporosis and by other diseases which affect the bones.
Osteoporosis
Osteoporosis is a bone disease which increases the risk of spinal fractures because it decreases the density of bone tissue. In osteoporosis, a fracture can occur with little or even no traumatic event. People who have severe osteoporosis may sustain a spinal fracture of the spine while carrying out simple activities such as picking something up from the floor or getting out of bed.
Sneezing or coughing can cause spinal fractures in these people. In cases of moderate osteoporosis, increased trauma is usually needed to cause a vertebral compression fracture, such as trying to lift something heavy. A fall may cause a spinal fracture in a person with moderate osteoporosis.
Osteoporosis typically occurs in women who have gone through menopause, but elderly men are also at risk, as well as people who have used steroid medications, like prednisone, over long periods of time.
Trauma
People whose bones are healthy generally sustain compression spinal fractures of the spine with severe traumatic accidents, such as sports injuries, motor vehicle accidents, or in hard falls in which they land on their buttocks or their feet.
Pathologic spinal fracture
A pathologic fracture is one that occurs because of a preexisting condition or disease at the site of the fracture. Most of the time, this type of compression fracture of the spine occurs due to a bone tumor. Cancer can spread from sites such as the lungs, breast, or prostate to the bone and destroy part of the vertebra. The compression fracture of the spine then occurs in the bone that has been weakened by the tumor.
Metastatic disease
The term metastatic is used to describe a condition where cancer cells spread to other parts of the body. The spinal bones are known to allow different types of cancer to spread to the body. A spinal fracture which happens without any apparent reason can be a sign of cancer spreading through the spine. Cancer can destroy some parts of the spinal bones, weakening them to the point where they collapse. Such spinal fractures are a clear indication that there is something happening internally which is causing harm to the bones.
Other conditions can also lead to pathologic spinal fractures and compression fractures of the spine, such as bone infections (osteomyelitis) and Paget's disease.
However, there are some underlying risk factors which can also lead to spinal fractures, that is if they go unchecked. There are two groups of people who are at the risk of developing spinal fractures.
These include:
-
- - Osteoporosis patients
- - People with cancer which has spread to their bones.
People diagnosed with some types of cancer, including multiple lymphoma and myeloma should be monitored for signs of spinal fractures, but a spinal fracture can be the first indication that an individual has cancer.
However, some people are at a higher risk of developing spinal compression fracture because of:
-
- Race – both Asian and white women have a higher risk of developing the condition.
-
- Age – the chances of spinal fractures are higher for elderly women.
-
- Weight – thin people are at a higher risk of fracturing their spinal bones.
-
- Early menopause – any woman who undergoes an early menopause has a higher chance of getting osteoporosis.
- Smoking – smokers lose their bone thickness faster compared to nonsmokers, and this puts them at risk of spinal compression fractures.
Prevalence
Spinal compression fractures occur most commonly in people who have osteoporosis. They affect about 750,000 people each year. An estimated 25% of all women past the age of menopause in the United States suffer from compression fractures of the spine. It is estimated that 40% of women who are at least 80 years old have the condition. It also affects men. The prevalence of compression fractures of the spine increases with age.
In the US alone, close to 10 million people have osteoporosis, and it is estimated that 34 million people are affected by low bone mass and they are at a higher risk of developing compressed fractures of the spine. 80% of the 10 million Americans affected by osteoporosis are women and 20% are men. The mortality rate for women with spinal fractures is 15% higher compared to those without the fractures.
Research has shown that people who have ever suffered a spinal fracture because of osteoporosis are very likely to develop a second spinal compression fracture. These spinal fractures can still be present in an individual but show no symptoms or minor symptoms. However, the individuals are still at risk of developing additional compression fractures to their spine.
Although the prevalence of compression fracture to the spine is very low in elderly men, the condition poses a significant health concern for them. In the US, the age group of elderly men aged 65 and above is growing very fast, meaning, the prevalence rate of spinal fractures in this group is likely to increase.
The prevalence rate of spinal fractures caused by osteoporosis is very high among white women as statistics show that 50% of these women will sustain a fracture at some point in their lifetime. Spinal fractures caused by osteoporosis are said to affect women 6 times more than they affect men. Osteoporotic spinal fractures to the spine have very adverse effects on the elderly as they are the main causes of disability and related injuries.
Estimates show that there are 550,000 spinal fractures related to osteoporosis every year in the US and 120,000 spinal fractures in the UK every year. Also, statistics indicate that there were approximately 1.4 million compression fracture cases in 2002 and most of these cases were reported to have happened in Europe.
Relevant materials:

The primary clinical symptoms of a compression fracture of the spine usually include one or more of the following:
- - Pain in the back, usually in the lower back, that appears suddenly
- - Walking or standing usually intensifies the pain
- - Lying down usually relieves the pain somewhat
- - Limited movement in the back can be a symptom of a compression fracture of the spine
- - Loss of height
- - Disability and deformity
If symptoms such as muscle weakness, tingling or numbness are present, this could mean the compression fracture of the spine is pressing on the nerves at the site of the fracture. If there’s bowel or bladder incontinence, or the person is unable to urinate, it could be that the compression fracture of the spine is causing pressure on the spinal cord and immediate medical attention should be sought.
Compression fractures of the spine sometimes do not cause any pain or other symptoms. Even in the absence of pain, if an elderly or middle-aged person develops a loss in height, a spinal deformity or has loss of mobility in the spine, they should be concerned about potential compression fractures of the spine. Women past the age of menopause should be especially concerned.
Patients that have compression fractures of the spine because of osteoporosis usually experience sudden pain in their backs. Most of these patients say that the pain begins immediately after engaging in a normal activity which slightly strains their backs. Some of these activities include:
- - Lifting light objects such as grocery bags
- - Opening a high window
- - Bending, like when tying their shoelaces or picking up something from the floor
Advanced osteoporosis can cause compression fractures of the spine for a person engaged in minor activities like coughing, sneezing or even turning over when sleeping. Pain caused by the osteoporotic compression fracture of the spine generally lasts for about 6 weeks as the affected bone heals. After 6 weeks, most patients complain about the severe pain turning into prolonged or chronic pain or an achy pain concentrated around the area where the compression fracture of the spine happened.
The pain usually subsides after a few weeks. In some rare cases, it can continue for months. Furthermore, some people complain about experiencing back pain even after the fractured bone is healed. This pain is mostly caused by long periods of inactivity.
Multiple compression fractures of the spine change the spine a great deal. The fractures mean that the vertebrae cannot support the weight of the spine, and can cause the vertebrae to collapse, resulting in some debilitating effects on the patient’s body.
Symptoms of multiple compression fractures of the spine include:
-
- Loss of height – every vertebrae fracture causes the spine to become shorter and a person can look shorter after several bones have collapsed.
-
- Kyphosis – vertebrae tends to form a curved shape after collapsing, causing the spine to bend forward, hence forming a curved back.
-
- Stomach problems – your stomach can be compressed by your spine if it gets shorter. As a result, you may begin experiencing digestive problems, such as a weak appetite and constipation, and you may begin to lose weight.
-
- Pain in the hips – if the spine becomes shorter, it pulls your rib cage closer to the hip bones. Pain can eventually develop if the bones begin to rub against each other.
- Challenges in breathing – the lungs can fail to function properly if the spine has been severely compressed. As a result, an individual may begin to experience challenges when breathing.
Diagnostic procedures
Medical history
Diagnosing a compression fracture of the spine starts with your doctor taking your complete medical history, your family's medical history, and a history of your current condition. You will then be given a physical examination to determine what is causing your symptoms.
Also, the doctor may ask if you are on medication for other medical conditions. Some medications cause the depletion of calcium in our bones, hence causing them to become fragile.
Physical exam
A thorough physical examination of your spine can help to reveal if there are any physical changes that show signs of a compression fracture. Compression fractures of the spine sometimes produce a notable bulge or projection at the affected area. At times, the spine can also bend forward or shorten as a result of a compression fracture.
Neurologic tests may be conducted for patients experiencing pain which radiates down their legs. These tests assist the doctor to determine the patient’s reflex and muscle strength and check whether there are compressed nerves in the fracture.
Imaging examination
Various imaging technologies can be used to get detailed information about the spine together with its surrounding soft tissues and nerves. The doctor can use these tests to see if there are signs of compression fractures of the spine. If there are signs of a compression fracture, the tests can help the doctor determine the severity and location of the compression fracture. These tests are very important, as they can help in estimating the time when the fracture happened.
If your doctor suspects a compression fracture of the spine, you will be tested for sensitivity and tenderness in and near your spine. Based on your medical history and the physical examination, an X-ray may be taken to confirm the diagnosis.
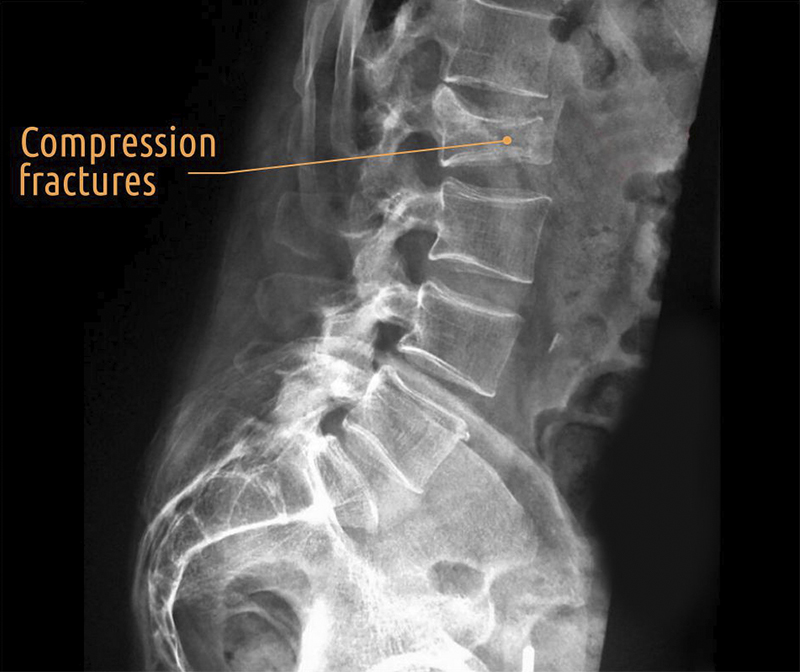
More often than not, if a hip or wrist is fractured due to osteoporosis, this is easily detected by an X-ray, but a compression fracture of the spine can sometimes be difficult to see on an X-ray. If the fracture is missed, one likely explanation may be that your pain is due to a muscle strain or arthritis.
In order to rule out other conditions, and depending on your doctor's findings from your X-ray, your medical history, and physical examination, additional tests may be ordered including:
Computerized Tomography: A CT scan may be used to see if the compression fracture of the spine is stable, or if it is affecting the nearby nerves. A CT scan provides cross-sectional views of the spine and surrounding structures.
Magnetic Resonance Imaging: An MRI can show the nerves and discs around the compression fracture of the spine in great detail and it can help rule out other causes of your symptoms, such as a herniated disc.
Nuclear Bone Scan: This test is useful in determining the age of a compression fracture of the spine to help determine the best treatment.
Bone density test: Also known as DEXA, bone density tests help to determine the levels of calcium and other important minerals in your bones. The scans are also used to check the quality or density of your bones. Once the images are received, they are processed and then converted into numeric values. These values are used to make comparisons between the bones of the patient who have the compression fracture of the spine and bones of healthy people.
Compression Fracture Treatment
When a compression fracture of the spine occurs, the fracture itself needs to be treated, as well as the osteoporosis that was responsible for the fracture. Compression fracture treatment typically involves conservative care such as:
-
- Rest: Most patients are most comfortable lying on their back. Bed rest assists in reducing acute pain in the back, but doctors say that it causes additional bone loss, thus worsening osteoporosis and increases the chances of getting more compression fractures.
-
- Pain relief: Non-steroidal, anti-inflammatory drugs (NSAIDs) like naproxen and ibuprofen are usually recommended for compression fracture treatments if tolerated. When the pain of a compression fracture of the spine is very severe, narcotics such as hydrocodone may be needed.
-
- Muscle relaxants: These reduce muscle spasms and help to control pain and serve as a compression fracture treatment. Examples include cyclobenzaprine and diazepam.
-
- Applications of ice or heat: These provide localized pain relief of a spinal fracture and compression fracture treatment.
- Back bracing: Back braces are used as a compression fracture treatment of fractured vertebrae. A back brace supports the fractured vertebrae externally, thus limiting its motion. The back brace is usually very rigid, significantly limiting motions of the spine. This helps in reducing pain. However, the patient should avoid wearing elastic braces because they don’t work. Additionally, the use of braces should always be supervised by a qualified physician.

- Physical therapy: A patient can join a rehabilitation program or start consulting a physical therapist once he or she starts to feel better. Further compression fractures can be easily avoided through exercises that strengthen the back. Some of these exercises include dancing, yoga and walking. They are very good options for a compression fracture treatment.
Sometimes surgery is recommended as a compression fracture treatment. The most common procedures performed for compression fractures of the spine are kyphoplasty and vertebroplasty. These minimally invasive procedures aid in healing the fracture.
-
- Kyphoplasty: This is designed to reduce the pain of a compression fracture of the spine. It stabilizes the bone and helps to restore the height of the vertebra using special instrumentation such as screws or rods. This procedure involves the following steps:
- Vertebroplasty: This surgery reduces pain in compression fractures of the spine. Under high pressure, special cement is injected into the affected vertebra to stabilize it.
Spinal fusion surgery
This surgery is another compression fraction treatment. It is performed to spinal compression fracture patients to reduce motion between two spinal bones and ultimately reduce pain. The surgery holds two or more spinal bones together, holds the bones in the right position and prevents them from moving until they fuse.
During the surgery, surgeons place metal screws into the vertebrae. These screws are joined to metal rods or metal plates which are attached to the back of the spine. The main purpose of the screws and the metal plates is to hold the spinal bones in place. Consequently, vertebral movement stops, giving the vertebrae a chance to join.
However, doctors say that this compression fracture treatment is usually the last resort. It’s recommended for patients with bones which have been compressed more than 50% in height, patients experiencing a lot of pain, or a patient who has had complications as a result of another spinal surgery.
Useful advice
If a patient has suffered one compression fracture of the spine, they are at an increased risk of further spinal fractures. This makes the compression fracture treatment of the underlying osteoporosis a very vital part of the overall back fracture treatment plan.
Osteoporosis prevention and treatment includes taking the following steps:
-
- Eating healthy: A well-balanced diet can help decrease your risk of spinal fractures.
-
- Get regular weight-bearing exercise. This increases bone strength
-
- Avoid smoking. Discontinuing smoking can help decrease your risk of spinal fractures.
-
- Take vitamin D and calcium supplements if you are at risk for osteoporosis
-
- Other medications: Women who are past the age of menopause may want to consult with their physician about estrogen replacement therapy. Other medications are also now available that are effective in reducing the risk of osteoporosis. Taking these medications may also decrease your risk of spinal fractures.
- If you take steroids for other medical conditions, talk to your doctor about the possibility of decreasing your dose to reduce the risk of spinal fractures.
A compression fracture of the spine caused by our lifestyles is avoidable. There are preventive measures and compression fracture treatments which can assist an individual to develop a strong back in their early ages. However, it is not all lost for you if you didn’t take some of these measures when you were younger. There are still things you can do to prevent spinal fractures. Here are a number of tips to consider:
-
- Exercise – exercise is one of the most helpful compression treatments out there. It will help you develop strong bones. Engaging in exercises, especially strength training and cardiovascular exercises at least three times a week can assist and tackle bone loss. Strong muscles will help you maintain or improve your balance. This, in turn, assists in preventing falls and other incidents.
-
- Stay hydrated – keep your body hydrated by drinking eight glasses of water every day. Water assists in reducing stiffness and improving the health of the spine.
-
- Maintain good posture – A neutral spine is the basis of good posture. A neutral spine helps to keep the spine’s natural curves in proper balance. Good posture keeps the bones correctly aligned and removes extra stress on the musculoskeletal system, allowing the muscles, ligaments, and joints to function properly.
- Avoid falls as much as possible – weak bones can easily break from even minor falls.
Therefore, you should take the following steps to prevent incidents which can make you fall:
- - Remove rugs which can make you slip and fall
- - Ensure that all the hallways and pathways are clear
- - Put skid-proof materials on the back of your rugs
- - Always use non-skid rubber mats in the bathrooms.
If you have chronic back pain and suspect it may be due to compression fractures of the spine, seek an appointment with your doctor. An accurate diagnosis and comprehensive back compression fracture treatment plan can help prevent significant deformity and other risks to your health that are related to multiple spinal fractures.






