Degenerative Disc Disease

What is degenerative disc disease? Degenerative disc disease or degenerative disc disorder, sometimes called DDD, occurs when one or more of the discs that lie between the vertebrae of the spine begin to dehydrate, shrink or compress. The condition mostly occurs in the cervical spine or lumbar spine. It can be very painful and can have a tremendous impact on the quality of life for people who develop the condition. Discs begin to degenerate as a normal part of aging and for many people, this doesn't cause problems. But in other people, degenerative disc disease that is not treated causes severe and on-going neck or back pain. It can also cause the following conditions:
-
- Osteoarthritis – this condition causes the cartilage which cushions and protects joints to break down.
-
- Herniated disc – the abnormal swelling or bursting or spinal disc.
- Spinal stenosis – it is the narrowing of the open space inside the spine which holds the spinal cord.
If unchecked, these conditions can apply pressure on the nerves and spinal canal, resulting in severe pain. In addition, these conditions can affect nerve function or even cause nerve damage.
In order to understand the definition of what degenerative disc disease is and what happens when an intervertebral disc breaks down as a result of the condition, it's helpful to know a little about how the spine works. Your spine is a structure made up of bones lying in a column. The bones of your spine are called vertebrae. One bone is a vertebra. Lying between each of these bones is an intervertebral disc. These discs can be affected by degenerative disc disease. They are filled with a gel-like substance, and they act like shock absorbers. They also keep your vertebrae from rubbing against each other. Sometimes discs are compared to jelly doughnuts. They have an outer wall, called the annulus, which is hard and tough, and the center called the nucleus, which is soft. For the most part, the discs are made up of water. As you age, or as you suffer from conditions like degenerative disc disease, the discs slowly dry out and shrink. As this process takes place, they lose their capacity to act as cushions for the vertebrae.
Furthermore, the spine has facet joints, which are located on the backside of the vertebrae. These joints function like the other joints in your body; they enable movement and play a very critical role with regard to the flexibility of the spine.
These joints are covered by cartilage, which acts as a protection to the bones when you are in motion. The bones can rub together without the cartilage. This can lead to very severe pain. Unfortunately, the general wear and tear of the spine can affect the cartilage, ultimately causing it to become worn out. As a result, osteophytes or bone spurs can develop as the body attempts to repair worn out bones.
The back has muscles, tendons, blood vessels, and ligaments. Muscles are the strands of tissues which assist in movement. Ligaments, on the other hand, are the strong and flexible fibrous tissues which link the vertebrae together and tendons join the muscles to the bones. Blood vessels offer necessary nourishment to the spine. All these parts work together to assist in movement, but can also be affected by degenerative disc disease.
Prevalence
So, what causes degenerative disc disease? Degenerative disc disease and disc degeneration are very common. In fact, 90% of people over the age of 60 have degenerated discs in their spine. However, most people do not have any symptoms of disease related to these degenerative changes that are part of the normal process of aging.
However, degenerative disc disease is not only for the elderly. Doctors say that disc degeneration affects the young and the old alike, sometimes at very rapid rates. Over time, most of these individuals start developing pain and other symptoms related to degenerative disc disease.
Data from healthcare facilities that treat disc degeneration cases show that the disease often leads to radiculopathy, or sciatica, which causes neural compression. In some cases, where the symptoms become chronic and unresponsive to medication, the patient may experience permanent disability, chronic pain and reduced quality of life. However, these cases are few because, in the majority of cases, disc degeneration is manageable.
Degenerative disc disease can cause low back pain known as discogenic pain, although the main cause of low back pain cannot be easily identified in some patients. 75% to 85% of people usually experience low back pain at some point in their lives at a prevalence rate of 15% to 45%. Doctors say what causes degenerative disc disease is not yet known and disc degeneration accounts for the majority of cases in chronic low back pain.
Even though low back pain is strongly linked to degenerative disc disease, not all patients who have shown radiological evidence related to degenerative disc disease, or disc aging will experience low back pain.
Degenerative disc disease rate of occurrence:
- Chronic low back pain is the most commonly reported problem and symptom related to degenerative disc disease. Close to 20% of all people with chronic low back pain as a result of degenerative disc disease are over the age of 65.
- Statistics show that close to 18% the world’s population will experience low back pain, even though it might not be related to degenerative disc disease.
- Degenerative disc disease can affect anyone and at any age, but it is most prevalent in people over the age of 60
- Doctors say that discogenic pain which is caused by degenerative disc disease accounts for the largest low-back pain cases.
- Data collected by Medicare between 1991 and 2002 indicates that there is a 132% increase in low back pain incidences as a result of disc denervation.
- The lifetime prevalence of degenerative disc disease is between 58% to 84% in the US labor force and accounts for most of the lost working days per year.
Risk factors
Individuals suffering from degenerative disc disease usually experience back pain, which radiates to the thighs and buttocks. At times, the pain can become worse if they bend, lift or twist. The pain occurs periodically.
Even though disc degeneration is a normal process of aging, certain factors can cause the condition to occur more rapidly. These factors include:
- Age: As we grow old, wear and tear on the intervertebral discs can cause neck and back pain. This is a common symptom of degenerative disc disease. So, people over the age of 40 are more likely to experience disc degeneration than younger people. People aged between 30 and 60 are at risk of developing degenerative disc-related disorders, whereas individuals aged 60 and above are in the risk of developing back pain as a result of degenerative disc disease. Therefore, chances of developing degenerative disc disease increase with age.
- Family history: Statistics have shown that some types of spinal disorders like degenerative disc disease are hereditary. Therefore, if a close relative, such as a parent or sibling had degenerative disc disease, your risk of developing the condition may be higher.
- Smoking: Smoking damages the blood vessels which the intervertebral discs depend upon for nutrients thus put an individual at an increased risk of developing degenerative disc disease. In addition, smoking produces free radicals, which can result in further disc damage.
- Diabetes: There has been a close association between diabetes and certain conditions like lumbar spinal stenosis, which can lead to disc degeneration. Therefore, diabetics have a higher probability of developing the condition
- Certain Jobs: Jobs that require prolonged driving, chronic vibration or heavy, repetitive lifting place increased stress on the spine and increase the risk for degenerative disc disease. In addition, jobs that require long hours of standing without resting, repetitive bending or sitting for long hours on a chair which doesn’t offer the necessary support to the back puts the individual at a greater risk of developing this condition.
- Sedentary lifestyle: Inactive lifestyle affects our backs as it makes them become stiffer, which can have an effect on the intervertebral discs, thus increasing the chances of developing degenerative disc disease.
- Excess weight: Excess weight increases pressure on the spine as it attempts to support the weight. Consequently, overweight people end up having damaged intervertebral discs which increase their risk of developing degenerative disc disease.
- Poor posture: Any form of persistent poor posture will, over time, increase the chances of developing back pain. Back pain can be caused by degenerated discs, which means people with prolonged poor posture are at the risk of developing the condition.
Causes of Degenerative Disc Disease
Physicians don't precisely know what causes degenerative disc disease, but several factors contribute to the condition. Most of these conditions come with symptoms of degenerative disc disease. They include:
- Age – As we grow old, our spinal discs begin to degenerate or break down, which can often lead to degenerative disc disease. The following are some changes which happen on the spinal discs as a person grows old.
- Loss of spinal disc fluid – this makes the discs less flexible and also affects their ability to act as shock absorbers. Loss of the fluid also causes the discs to become thinner and narrows the space between the spinal bones.
- Small cracks or tears in the outer layer of the discs – the jelly-like materials inside the discs can be forced out through the cracks or tears in the disc. As a result, the disc can swell, rupture, or break into small fragments.
- Cigarette smoking - Cigarette smokers are at an increased risk of suffering from degenerative disc disease, especially as they age. The risk is even higher for chain-smokers.
- Traumatic injuries
- A sudden trauma or injury to the spine which can be a result of falls or car accidents can cause herniated discs, which are known to begin the disc degeneration process.
- Unstable Spine: As the space between the vertebrae becomes smaller, the padding between them begins to decrease, hence making the spine less stable. The body generates more bones in order to stabilize the spine and this leads to osteophytes or bone spurs, which in turn leads to degenerative disc disease.
Other factors include:
- - Arthritis
- - Osteoporosis
Degenerative disc disease is thought to be a cause and effect cascade or process. One change occurs, which causes more degeneration and changes in the structure of your spine. When these changes are combined, they cause the emergence of degenerative disc disease symptoms or the disease itself. Degenerative disc disease starts with changes in the intervertebral discs and then proceeds to affect other moving parts of the spine, like the facet joints. Over time, the collagen structure of the outer part of the affected intervertebral disc begins to change. Then, the fluids which assist movement in the discs decrease. These changes affect the discs ability to support the spine and handle back movements.
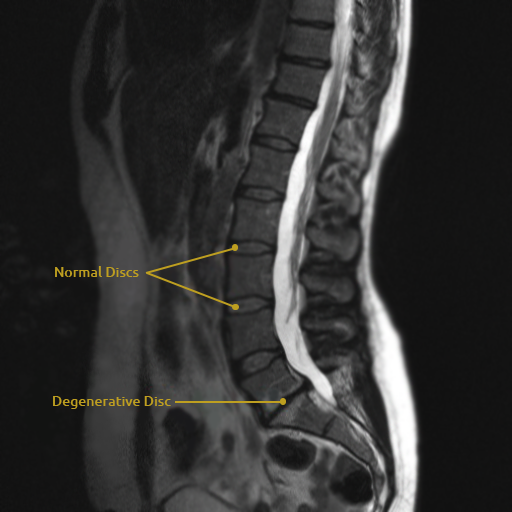
Most disorders that relate to degenerative disc disease can be detected by an MRI. This is an imaging test that shows the different parts of the spinal column and back very clearly. It's interesting to note that many people who have back pain have abnormalities that can be clearly seen on MRI studies. But nearly one-third of young adults who are healthy and have no pain also have these same abnormalities, such as degenerative disc disease. This is according to MRI studies of their spine.
It is unknown why some individuals experience pain related to symptoms of degenerative disc disease while others do not.
Read also:
Degenerative Disc Disease Advice: Yoga, Dieting, Posture, & Care
The degenerative disc disease can affect any part of the spine. However, it mostly affects the cervical spine and lumbar spine. Most people will experience pain which is one of the most common and obvious symptoms of degenerative disc disease. The area at your back from which your back pain erupts will most likely be the location of the damaged disc.
In some cases, pain can also be traced to other body parts. The nerves branching off your spine travel to different parts of the body, and if the degenerative disease affects a nerve in the upper back, you might experience pain in your hands.
Chronic neck or back pain is the main symptom of degenerative disc disease. The pain can flare up at times, and doctors call that an acute episode. Although the main symptom of degenerative disc disease is the pain, you should always monitor its occurrences and what relieves it or makes it worse.
At times, individuals with degenerative disc disease can notice the following pain patterns:
- - More pain when they sit for long periods of time, or when lifting, twisting or bending.
- - Reduced pain when running or walking.
- - Less pain when they change positions regularly.
- - Less pain when they lie down
These patterns will be experienced in either the neck or lower back. But a person should also watch out for the following symptoms of degenerative disc disease:
-
- - The pain that occurs is usually activity-related. It will be worse at times, but then decreases to a lower level of pain or will go away entirely.
-
- - Episodes of severe pain in the neck or back that most often last from a few days to several months before the individual returns to his or her usual levels of chronic pain.
-
- - The individual's baseline level, or level of chronic pain they typically experience, varies significantly among patients who have degenerative disc disease. It can range from almost a zero level of pain or just a nagging sensation to very severe, sometimes debilitating pain.
-
- - While degenerative disc disease can cause debilitating chronic pain, these cases are extremely rare.
- - Certain activities cause the pain of degenerative disc disease to aggressively intensify. These activities include twisting, bending, lifting and other such motions.
-
- - Certain positions also intensify the pain of degenerative disc disease. For instance, if the lumbar discs are involved, sitting will almost always make the pain worse. This is because of sitting places a three times greater load on the lumbosacral discs than standing.
-
- - In most cases, walking is more comfortable than sitting for people with degenerative disc disease. Even running can sometimes feel better than extended periods of standing or sitting.
-
- - Changing positions frequently usually helps patients with degenerative disc disease feel better.
- - Lying flat on their back is not usually comfortable for individuals with degenerative disc disease of the lumbar spine. It is generally more comfortable for them to lie with their legs propped up or with a small pillow under their knees. This helps to remove the pressure from the lumbar disc space and relieves some of the pain caused by degenerative disc disease.
Diagnostic procedures
Many people do not know what a degenerative disc is, yet a good number of them will have to deal with it at one point in their lives. When you first start having pain and symptoms of degenerative disc disease, notify your family healthcare provider. Your physician will obtain your medical history. This will help him to better understand any other medical conditions you might have, any prior traumatic injuries and your current symptoms of degenerative disc disease. He will also be able to determine if any factors in your current lifestyle are contributing to your symptoms of degenerative disc disease.
During a degenerative disc diagnostic procedure, the doctor will typically ask the following general questions:
-
- When did you first start experiencing the neck or back pain?
-
- Which kind of activities were you recently engaged in?
-
- Have you taken any measures to control the pain?
-
- Is the pain located in one area, or it also travels to other parts of the body?
- Does anything reduce or worsen your pain?
Your doctor will also complete a physical examination as part of the process towards determining the root cause and source of your pain.
An examination almost always includes tests for muscle weakness and tests for your reflexes. Your physician will also check for any numbness or changes in sensation to help diagnose, or rule out degenerative disc disease and other serious disorders.
In addition to obtaining your medical history and performing a thorough physical examination, your physician may order imaging tests to identify conditions that may be causing pressure on your nerve roots and leading to symptoms of degenerative disc disease. These tests include:
-
- X-rays take images of the bones and can be helpful in determining what is causing symptoms of degenerative disc disease like those associated with degenerative disc disease.
-
- MRI scans are sometimes recommended if a physician suspects degenerative disc disease.
-
- Myelogram – this test assists the doctor to determine if the patient has a spinal cord or spinal canal disorder, or whether it is nerve compression that is leading to weakness and pain. During the test, a special type of dye is injected into the part around the nerves and spinal cord and then a CT scan or X-ray images are taken. These images give a complete anatomic picture of the spine, particularly of the bones. These images assist the doctor to know if there are any abnormalities in the spine. The test is sometimes used to rule out other conditions associated with degenerative disc disease.
-
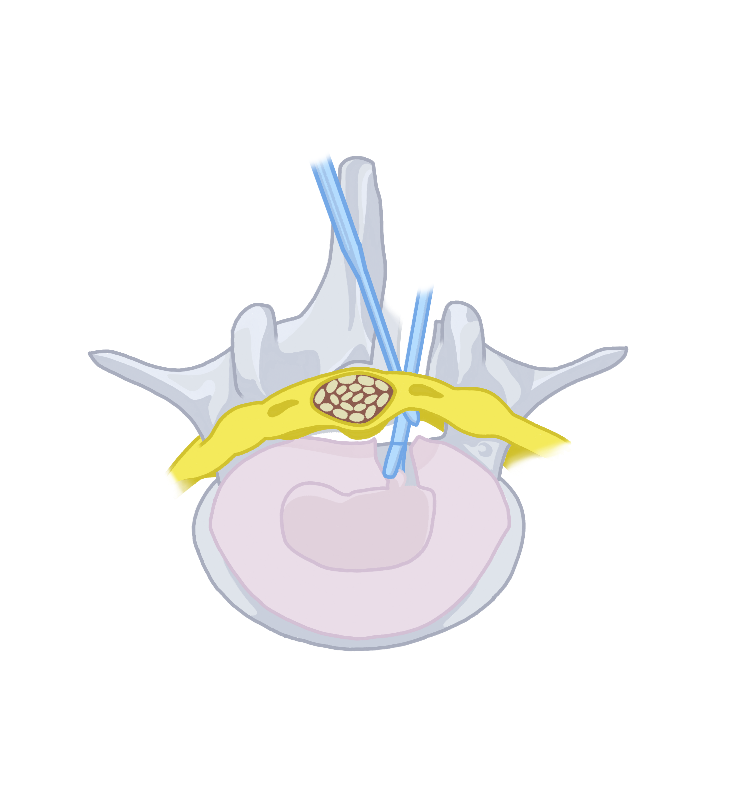
- Discogram or discography – the doctor can use discography to confirm whether the discs are the source of a patient’s pain. A harmless dye is injected into the suspected discs and if the disc has a problem, the dye is expected to leak out of the disc.
- CT scan – CT scan is usually more effective compared to X-ray as it can assist in identifying issues like herniated or protruding discs. The scan can be very helpful, as it can easily show both the bone and nerves, essentially assisting the doctor to see if a bone spur is causing pressure on the nerve.
- Bone scan – a bone scan can be conducted to check for the presence of spinal problems like fractures, infections or osteoarthritis, which are mostly related to degenerative disc disease.
Depending on the results of these tests, your doctor may refer you to an orthopedist, neurologist or a neurosurgeon for further treatment of the degenerative disc disease.

Treatment for degenerative disc disease will either include conservative or surgical treatment methods. Conservative treatment for degenerative disc disease includes interventions such as back school and back education, medications and exercise, injections and physical modalities.
Back School and back education
This is one of the treatments for degenerative disc disease. The goal of back school and back education is to teach individuals who have back pain associated with degenerative disc disease how to help themselves manage their symptoms. Typically, the first topics covered are the anatomy of the normal spine, basic biomechanics and the mechanisms of back injury. Following these subjects, spine models are used to explain the diagnosis of degenerative disc disease to the patient and find the appropriate treatment for degenerative disc disease.
Throughout the course, patients are taught basic body mechanics and correct posture for completing tasks of daily living, such as:
- - Standing and sitting
- - Standing at a drawing board or beside a desk
- - Brushing teeth and washing of hands and face
- - Pulling, pushing and lifting a weight to prevent further injury and pain related to degenerative disc disease
- - Getting into and out of bed and sleeping
- - Getting into and sitting in a car
Patients are also taught the correct and incorrect methods of lying down, sitting, bending over, sneezing or coughing during episodes of acute degenerative disc disease back pain. Knowledge is also a treatment for degenerative disc disease.
Exercise
Depending on each individual's diagnosis, different kinds of exercises may be prescribed for the treatment of degenerative disc disease. Different types of floor exercises may include:
- - Abdominal bracing to increase core strength
- - Double-knee-to-chest
- - Modified sit-ups
- - Seat lifts
- - Low back stretches to increase flexibility and strengthen muscles as a treatment for degenerative disc disease
- - Mountain and sag exercises
- - Hamstring stretches to increase flexibility and strengthen muscles
- - Knee-to-elbow exercises
- - Extension exercises
Heat and ice treatment
Applying heat to stiff joints and muscles can improve their flexibility as well as their range of motion, and serve as a treatment for degenerative disc disease. Ice packs, on the other hand, can cool down painful muscles, or numb the parts where the painful episodes are concentrated.
Manual manipulation
Spinal manipulation, like chiropractic manipulation, can assist in relieving pressure applied to sensitive tissues or nerves, thus reducing pain experienced in the low back area. In addition, spinal manipulation can restore blood flow, improve range of motion, reduce muscle tension and stimulate the release of endorphins, which are natural painkillers produced by the body.
A doctor can suggest spine surgery for a patient who fails to respond to conservative treatment for degenerative disc disease methods. The surgery is determined by where the degenerative disc disease has affected the spine. Common surgical procedures for the treatment of degenerative disc disease include:
-
- Facetectomy – the facet joints in your spine play an important role in stabilizing the spine, and they can also put stress on a nerve. During facetectomy, the surgeon removes the facet joint to relieve that pressure.
-
- Foraminotomy – this surgical procedure is done in cases where a bone spur or part of the disc exerts pressure on a nerve as it exits through the foramen. The surgeon makes the foramen’s opening larger, to allow the nerve to exit without being pressed.
-
- Laminectomy – every vertebra has a bony plate which protects the spinal cord and spinal canal. The bone plate is known as lamina. At times, this bone can compress the spinal cord, and a surgeon can remove a part of the entire lamina to create more room for the spinal cord.
- Discectomy – herniated or protruding discs can cause compression to your nerves. During discectomy, a surgeon removes a part, or the entire disc in order to relieve the pressure. This surgical procedure can be invasive, but very few incisions are made during the surgery.
Prevention
Since degenerative disc disease is mainly associated with the process of aging, it is impossible to prevent in every case. Following a healthy diet, making lifestyle modifications and adding exercise to your routine on a regular basis can help minimize, or even prevent painful and debilitating symptoms of degenerative disc disease. Therefore, our lifestyle can help prevent having to go for treatment for degenerative disc disease.
Exercise: Movement improves the body's circulation. That means blood flow increases to the muscles and organs. Blood carries oxygen along with healing nutrients and carries away waste products. This helps to preserve muscle function, as well as the function of the vertebral discs and the spine itself to minimize the possibility of having to go for treatment for degenerative disc disease.
Exercise also stimulates the body to release endorphins, the "feel good" chemicals in the brain and also helps to reduce pain. At least 30 minutes of moderate, low-impact, strength training exercise is recommended for people who have degenerative disc disease. Some of these exercises include swimming, biking or walking, and can maintain mobility and flexibility as well as control weight. These exercises can also be used as a treatment for degenerative disc disease.
Lifestyle modifications: This includes interventions like the following to delay wear and tear damage to the spine that is common in degenerative disc disease:
-
- Avoid smoking: smoking has negative effects on the health of your bones. The habit can accelerate the degenerative process, particularly in the spinal bones.
-
- Posture: Make sure you sit up straight, choose a chair with adequate lumbar support and armrests, and keep your feet flat on the floor, or use a footstool.
-
- Change positions frequently: especially if your job requires you to sit for extended periods.
-
- Use proper lifting techniques: This will save your back a great deal of trouble and minimize your risk of acquiring degenerative disc disease.
-
- Make sure you have a supportive mattress to sleep on.
-
- Maintain a healthy weight and stay well-hydrated: being overweight strains your body. In addition, the extra weight can put extra stress on the spine, and force the vertebrae and discs to work much harder to support the body and this can accelerate the generative process.
-
- Reduce alcohol intake: A reduction in alcohol intake will help decrease the risk of spinal conditions.
-
- Stretching: Five minutes of stretches every morning and evening before going to bed can significantly improve mobility. Hamstring stretches are mostly recommended for people experiencing lower back pain. In addition, more stretches, like piriformis stretches, which target the affected areas can be recommended, depending on the diagnosis results.
-
- Water aerobics: For people experiencing pain that is too severe to handle exercises, a gentle approach is the best way to go. Water therapy is usually very gentle for the lower back, as water supports the body weight.
- Eat healthily: A balanced diet can improve bone health and also strengthen your spine. Therefore, a healthy diet can prevent you from suffering from degenerative disc disease. In addition, drinking plenty of water assists to keep the spinal discs hydrated and flexible.
Many people usually have the misconception that degenerative disc disease affects the spine of all elderly people. However, if taken good care of, the spine can serve you well for many years without giving you any trouble, even in old age. So, if you handle your back well during your younger age, your spine won’t bother you when you grow old.
Pathological changes
Discs that are aged or degenerated usually contain fibrocartilage that is degenerated and they also show chondrocytes, which are cells that aid in the repair of damaged cartilage. This suggests that discs are being restored. It is a routine practice to examine disc fragments which are surgically removed to check for any possible malignant growth that may cause symptoms like those of degenerative disc disease. The practice also assists in finding the treatment for degenerative disc disease.
As vertebral discs age, the gel-like material in the center is replaced with fibrocartilage. The tough outer rim of the disc, becoming dry, is prone to split, crack or tear, and this allows the gel-like center material to leak or bulge out (herniate). The center of the disc can also shrink. This causes the outer rim to fold in or prolapse, and bone spurs then form along the edges of the vertebrae lying on either side of the disc. This is common in the degenerative process that occurs with degenerative disc disease.
Some of the potential complications of degenerative disc disease include spondylolysis, protrusion and/or subluxation of the vertebrae (spondylolisthesis) and spinal stenosis.
Studies have shown that most of a patient’s degenerated discs don’t always show symptoms. Some researchers have revealed that there is lumbar disc degeneration in at least 35% of people between 20 and 39 years but cases of disc degeneration are very evident in individuals aged between 30 and 80 years. However, it is increased to differentiate pathological degeneration from the normal aging process in patients showing degenerative disc disease symptoms.
The pathological characteristics of the discs for patients with discogenic pain show the development of vascularized granulation tissue and a widespread innervation extending. These conditions extend from the outer parts of the annulus fibrosus to the nucleus pulposus in the torn fissure of the annulus. There is, on the other hand, penetration of mast cells in the granulation tissue areas. Mast cells mostly lead to inflammation of disc tissue, fibrosis formation, neovascularization and degradation of disc tissue. All these effects contribute to the development of back pain.
Currently, there is still no clear distinction between the pathological disc degeneration and aging changes. However, MRI tests have led to a better clinical understanding of disc degeneration, including facet joint degeneration, annular tears, and loss of signal in the annulus and the nucleus.
Understating the pathological changes of degenerative disc disease can assist in finding a degenerative disc cure, and lead to the development of tissues to assist in the restoration of degenerated discs biologically. In the future, the best treatment for degenerative disc disease will be the one that will lead to total back pain eradication, as well as the biological reversal of the degenerative process. Furthermore, it is very critical to identify the pain patterns of degenerative disc disease as structural failure of the degenerated disc does not always relate to pain.






