Kyphosis
Kyphosis: Definition
Kyphosis is the medical term for "hunchback." It happens when the upper portion of the spine (the thoracic) region is abnormally curved forward. Some forward curvature in this region is normal, but if the curve is greater than 50 degrees the condition is considered to be "kyphotic" which is abnormal.
A common kyphosis definition states that kyphosis is a forward, exaggerated rounding or curvature of the back, usually the upper thoracic part of the spine which creates the appearance of a hunchback.
Kyphosis is most common among elderly women. However, it can affect anyone, regardless of their age. Its occurrence among elderly women is often a result of osteoporosis weakening their spinal bones, so much so that they compress and crack.
In instances where kyphosis affects a younger person, it is usually as a result of developmental problems, spine trauma and degenerative diseases like arthritis. Unlike severe cases of kyphosis that are often painful and sometimes can cause disfiguration of the back, mild kyphosis causes few manageable problems.
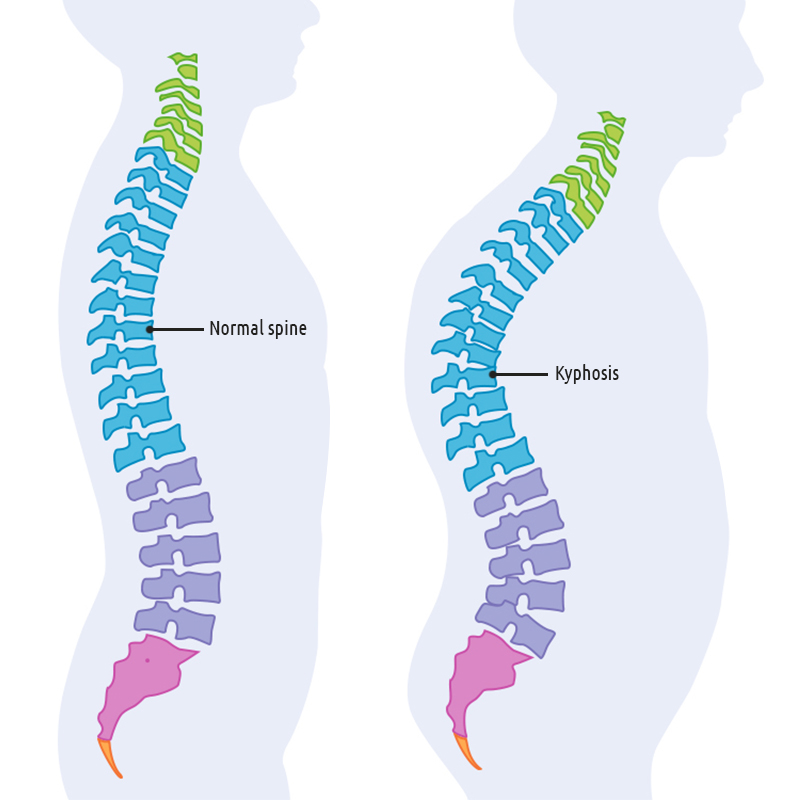
One interesting fact about the spine is that it’s made of a series of ordinary curves that play an important role in absorbing the weight that the body exerts on the spine. The cervical spine curves a little inward, the thoracic spine outward and lumbar bends inwards. Although the lower part of the spine carries most of the body’s weight, all the parts rely on each other to function normally.
Additionally, the curves make it possible for the head of a normal person to stay at a balance directly over their pelvis. However, the head may stay out of balance if the curves of the spine are abnormal. This can result in stiffness, changes in posture or walking pattern problems and back pain.
Scheuermann’s kyphosis, also known as developmental kyphosis is a form of kyphosis which happens during the developmental stages of a person. This condition is caused by stiffness in the vertebrae. At times, Scheuermann's disease adds extra abnormalities, known as Schmoll's nodes to the affected part of the vertebrae. Spine specialists say that the disease thickens and tightens the anterior longitudinal ligament, leading to spinal deformity.
The thickened ligament can have an effect on the growth of the vertebrae in young children and causes an imbalance in its growth. In most cases, there is less growth in the front of the vertebrae and too much on its back. As a result, a wedged vertebrae forms.
When viewed from the front, the spine has a straight look. However, there are some spines that can still show an abnormal curve even when viewed from the front. This condition can be caused by abnormalities of the spine during birth, growth abnormalities in the adolescence stage, unusual vertebrae twisting caused by muscle spasms, especially after an injury, and degenerative spinal changes that occur in adulthood.
Generally, any kyphosis definition has to include the rounding of the back. However, it is important to note that not all cases of a curved upper back are abnormal. Therefore, a good definition must emphasize the exaggerated nature of such a curve.
Prevalence
Kyphosis is thought to affect men and women equally, although this has been debated in some literature. The disorder affects approximately 4 to 8% of the overall population. However, we’ve also seen that kyphosis affects women more than men, specifically elderly women. Therefore, this is an important aspect of the condition, thus the reason why we include it when we define kyphosis.
Postural round back, or hyperkyphosis, is very prevalent in the western societies. Statistics show that the condition, which is very common, affects 15.3% of all Americans. It is also estimated that close to 40% of the elderly have hyperkyphosis, and are also at a higher risk of developing more adverse symptoms related to kyphosis. The prevalence of this condition increases with age, and the greatest change in curvature happens among women aged between 50 to 59 years.
A research conducted to determine the prevalence of kyphosis among school-aged children revealed that kyphosis mostly affected children attending private schools. The main cause of kyphosis among these children was the weight of their school bags.
The statistics showed that 36.9% of public school students and 55.1% of private school students carried backpacks which were not commensurate with their weight. The researchers concluded that there was a significant relationship between the standard weight of a backpack and the prevalence of kyphosis among students.
Regarding the relationship between kyphosis and gender, kyphosis is known to be more prevalent in women than in men. However, there is conflicting data regarding this relationship, as some studies have indicated that more men suffer from kyphosis than women. The researchers stated that the lower prevalence of kyphosis in women was because their working hours were 20% less compared to men. The study showed a significant relationship between gender, working hours and kyphosis.
However, there is a very high prevalence of kyphosis among women. Statistics show that 35% of all women aged between 20 and 60 years have kyphosis. There is also a substantial relationship between upright postural kyphosis and normal postural kyphosis index. In the case of postmenopausal women, normal postural kyphosis is said to be inversely connected to age. So, both upright postural kyphosis and normal postural kyphosis are not related to age in postmenopausal women.
Scheuermann’s kyphosis is prevalent in young people, especially teenagers. It is estimated that this condition affects around 8% of the population in the United States. In Europe, Scheuermann's kyphosis is said to affect 8% of people above the age of 50.
Some in the scientific community defines kyphosis by including its prevalence and symptoms. One of the lesser known cause of kyphosis is genetic disorders. The most common kyphosis caused by genetic disorders is congenital kyphosis. It is caused by abnormal vertebral development during pregnancy and it is normally identified after the child has been born. The prevalence of congenital kyphosis is very low, happening once for every 2000 births.
Risk factors
Spinal kyphosis is a disorder which can occur at any stage of life, but it is rarely seen at birth. In adolescents, the disease is also called Scheuermann's disease, and the causes of the condition, or what increases the risk of developing it, are unknown.
In adults, many different conditions can lead to the development of kyphosis, and each of these different causative conditions has their own risk factors.
Risk factors for kyphosis
- Old age – elderly people are more likely to develop kyphosis because of osteoporosis.
- Gender - Available research shows that women are at a higher risk of developing kyphosis than men.
- Teenage girls are at an increased risk of developing postural kyphosis because of poor posture.
- Vertebral fractures – these are different from arm or leg fractures as they mostly involve the spinal cord. The spinal cord is protected by the spinal column and any damage to the column can cause injury to the spinal cord. Some of these injuries are known to make the spine bend.
- Osteoporotic fractures – the spine is composed of small bones known as vertebrae. Weakness or fractures of these bones can make someone develop a hunched posture.
- Traumatic fracture – spinal fractures can be caused by car accidents or falls from a significant height. People with traumatic fractures to their spinal cords risk developing kyphosis if the fractures are not treated well and promptly.
- Osteogenesis imperfecta - also known as brittle bones, it is a rare condition which affects the connective tissue. People with this condition have very fragile bones, which can break or fracture very easily, mostly without any cause. Research has revealed that people with such a condition are at a higher risk of developing kyphosis.
- Myelomeningocele – this is a birth defect which happens during the early stages of fetal development and can cause kyphosis in a child’s back.
- Marfan syndrome – it is caused by a genetic mutation in the genes which allows collagen cross-linking. Patients with this syndrome have a unique appearance. They are tall, with long legs, arms, and fingers. These patients are mostly associated with scoliosis, which puts them at risk of developing kyphosis.
- Scheuermann disease – the disease is known to cause back pain, which can lead to long periods of inactivity. If not managed, Scheuermann disease can cause a rounded back, also known as kyphosis.
- Degenerative disc disease – it’s caused by wear and tear in the spinal cord over a long period of time. Anyone suffering from this disease is also at the risk of developing kyphosis.
All these risk factors can lead to spinal kyphosis. A person affected by one or more of these risk factors have a higher chance of getting kyphosis compared to a person unaffected by any of these risk factors. All the same, the fact that you are not affected by any of the risk factors in no way means that you are safe and can't contract kyphosis.
Reasons
Normally, the bones of a healthy spinal column (the vertebrae) are stacked one on top of each other, like cylinders, with intervertebral discs in between each pair. When the bones in the upper portion of the back begin to become shaped like wedges instead of cylinders, kyphosis occurs. This abnormal curve can be caused by several different problems or a combination of problems. Common kyphosis causes include:
- Osteoporosis: This is a disorder of the bones that can result in compression fractures of the vertebrae, or of any other bone; the thin and fragile bones are crushed or broken in the incident of a fall, accident or any injury, that can then lead to kyphosis. Osteoporosis most commonly occurs in older adults, especially post-menopausal women. People who have taken corticosteroids in high doses over long periods of time are also at increased risk for osteoporosis.
- Disk degeneration: The intervertebral discs lie between the individual vertebrae of the spine and act like shock-absorbers. As we age, these discs degenerate, meaning they become dry and shrink. This can cause increased problems with kyphosis.
- Scheuermann's disease: Scheuermann’s disease is responsible for causing kyphosis among young people. This is a disease that begins in adolescence, typically before puberty. It is also called Scheuermann's Kyphosis. It is more common in males than in females. The kyphosis may continue to worsen as the teen matures. The cause of the disease is unknown.
- Birth defects: If the spinal column does not properly develop while the fetus is in the womb, the vertebrae may not properly form and kyphosis may result. In some cases, two or more vertebrae join together. Doctors have not yet understood why this condition happens at this stage. However, scientists have discovered that this condition can run in families, and have stated that genetics play a role in such cases.
- Syndromes: Children sometimes develop kyphosis that is related to certain disorders such as Prader-Willi disease or Marfan Syndrome.
- Cancer and cancer treatments: The presence of a malignancy in the spine can create weakness and make the vertebrae more susceptible to injury and deformities such as kyphosis. Radiation treatments and chemotherapy also can weaken the bones of the spine and lead to compression fractures.
- Paget’s disease: this disease disrupts the development of new backbone cells, hence weakening the bones.
- Muscular dystrophy: a condition which leads to a progressive weakening of the back muscles. It is also said to be genetic.
- Spinal injuries are also known to cause kyphosis.
- Arthritis – it can cause inflammation of the joints in the spine. The inflammation can then make the spine to become rigid, creating spinal instability. Therefore, anyone suffering from the arthritis of the spine can develop kyphosis as a result of the spinal instability.
Postural kyphosis is a condition that is not related to any physical deformities. The increased kyphosis in the upper back, in this case, is caused by slouching, carrying heavy bags or leaning back in chairs. Postural kyphosis can make the muscles and ligaments which support the backbone to stretch. This can force the upper back to bend out of its normal position. It is most prevalent in teenagers.
Classification
There are several different types of kyphosis. They include:
- Postural kyphosis: This is the most prevalent kind of kyphosis. Slouching is normally believed to be the primary cause of the condition and young people, as well as the elderly, can develop it. In young people, it is generally a reversible condition that resolves when muscular imbalances are corrected. In older people, the disorder is sometimes known as a "dowager's hump." Approximately one-third of the elderly who have severe postural kyphosis have fractures of the vertebrae.
- Scheuermann's kyphosis: This disorder causes a more extreme physical deformity and it can also cause pain. It is also known as Scheuermann's disease. This condition can affect various areas of the spine but it most commonly affects the thoracic (upper back to neck) area. This type of kyphosis usually starts in puberty and is more common in boys. Patients with Scheuermann's kyphosis are physically unable to correct their posture. Portions of their spine, especially the thoracic vertebrae, are very stiff and rigid. These areas may be very painful and the pain increases with activity and also with extended periods of sitting or standing. This kyphosis can have a devastating effect on a teenager's life. They may feel uneasy around their friends or isolated and shamed, depending on the severity of the deformity. When comparing Scheuermann's to postural kyphosis, the vertebrae and discs are very different. In postural kyphosis, the structures appear normal. In this condition, the bones are misshapen, irregular and are often herniated. Probably because of the intense amount of muscle effort that is required to sit and stand properly, fatigue is a common symptom. Scheuermann's kyphosis seems to have familial tendencies. Most patients who undergo surgery because of their kyphosis have Scheuermann's disease.
- Congenital kyphosis: If kyphosis is present at the time of birth it is known as congenital kyphosis. It can occur as the result of problems with the development of the spinal column while a fetus is developing in the uterus (womb) of its mother. The vertebrae can be misshapen, or they can be fused together and this causes the kyphosis to progress further as the child grows. Sometimes surgery is needed very early to help prevent abnormal spinal curvature, and close monitoring is necessary to watch for changes. There are potential risks to the child, so the decision to proceed with the surgery for the kyphosis can be difficult. Sometimes congenital kyphosis is present at birth but does not appear until the child is older. This happens more frequently with children who have neurological disorders such as cerebral palsy.
- Nutritional kyphosis: This kyphosis occurs as the result of nutritional deficits, especially in childhood, that affects the bones. One example of nutritional kyphosis is the curving of the spine that results from a deficiency of vitamin D. This can cause rickets which results in soft bones. This not only produces kyphosis of the spine, it also can cause the bones of the limbs to curve under the weight of the child's body.
- Gibbus deformity: This type of kyphosis often occurs following an infection with tuberculosis. It can happen as a result of the vertebrae collapsing.
- Post-traumatic kyphosis: As the name implies, post-traumatic kyphosis is a disorder that can be the result of a serious accident or injury, for example, falling from a significant height, a car accident or a horseback accident. The impact of these events can cause dislocations and/or fractures of the spine or the spinal discs. Post-traumatic kyphosis can develop if these conditions are not promptly or properly treated.

Kyphosis: Symptoms
The most common kyphosis symptoms and the easiest to recognize is a rounded upper back. The extreme curvature of the upper spine causes a "humpback" appearance or causes the individual to hunch forward.
The changes to the spine are very gradual, and this makes it very hard for an individual to note the changes happening in their back posture and notice kyphosis symptoms. Mostly, it’s friends and family who note these changes before the individual. In other cases, an individual may notice a sudden change in their back posture. These situations demand the individual to seek immediate medical attention as a curved spine can be linked to other health issues.
Kyphosis symptoms are mostly seen in the early teens, especially between the ages of 10 and 15. It’s very hard to note the problems at their early stages as X-ray scans don’t show the changes until later. Typically, this condition is discovered by parents when they start noticing slouching or poor posture in their child. Otherwise, a teenager can start to experience mild pain and some fatigue in their mid-back. Unless the deformity is severe, the pain is rarely severe or disabling at these initial stages.
Scheuermann’s disease causes a rigid curvature or deformity to an individual. The curvature can worsen when the individual bends over and then corrects itself once the individual stands straight. A person starts experiencing pain after having the deformity for a long time.
In addition to this, other kyphosis symptoms can include:
- - Mild to severe pain in the back, especially with movement
- - Extreme tiredness or fatigue
- - Stiffness and tenderness of the spine
- - Forward positioning of the head
- - Unequal shoulder height
- - Muscle tightness in the back of the thighs (hamstring muscles)
- - In severe cases, breathing may be difficult or chest pain may occur
- - Walking slowly
- - Challenges in breathing, especially in the more severe cases
Diagnostic procedures
If you have kyphosis symptoms, your doctor will most likely perform a routine physical examination including finding out how tall you are. The examination assists the doctor to know the patient’s progress in the entire treatment period. In addition, physical examination will assist the doctor in understanding how to fix kyphosis depending on its location and factors.
Physical examination includes:
- Observation – the doctor may observe your posture to see if there are signs of gibbus or round-back deformity. Assessments can be done to determine the balance of the head and the body over the pelvis. If you have any related scoliosis, it will also be observed.
- Adam’s forward bending test - You may be asked to bend forward at the waist so the doctor can see your spine from the side. Thoracolumbar kyphosis symptoms are easily revealed by this test. The development of kyphosis symptoms may be easier to view from the side.
- Palpitation – the doctor uses his hands to check for the presence of any spinal abnormalities. Scheuermann’s disease makes the hamstring muscles tight, something that this test easily shows.
- Range motion – a physician uses this test to determine the extent to which a patient can perform certain movements like extension reach, spinal rotation, and lateral bending. The doctor will then assess the rigidity or flexibility of the curvature.
- Neurologic evaluation - Your physician may also do some simple neurological tests to check your muscle strength and reflexes. Evaluations are also done to check the following kyphosis symptoms: paresthesias, numbness, bowel or bladder changes, motor function, and extremity sensation.
Your physician may recommend you for further testing, depending on the severity of the kyphosis symptoms and signs. Some tests your doctor may order include:
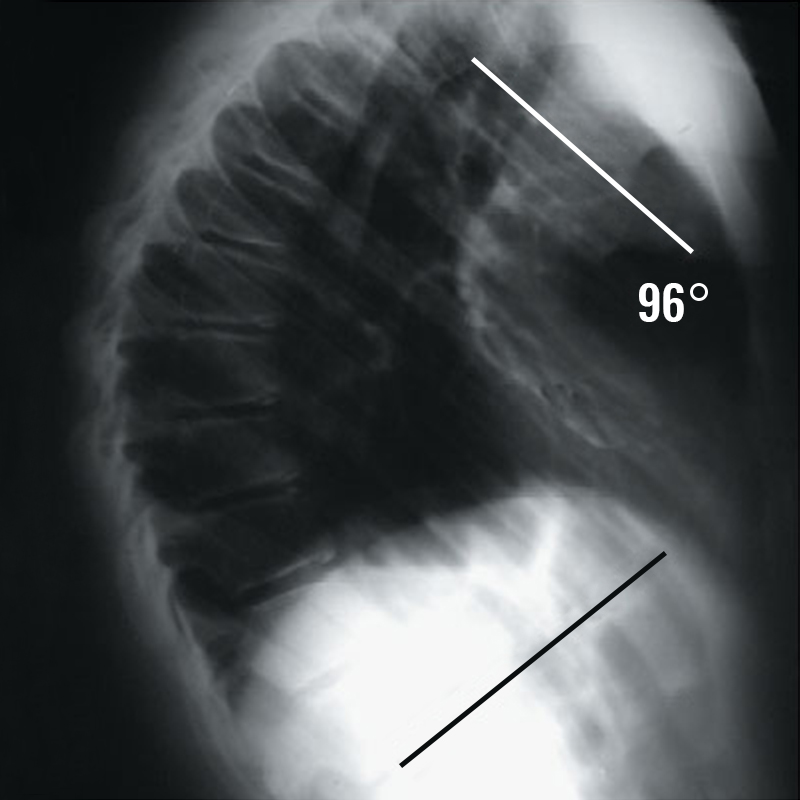
- X-rays: Simple X-rays can help determine how severe the kyphosis is. They can also detect some abnormalities in the vertebrae and this can help discover what type of kyphosis you have.
- Computerized tomography (CT scan): If your physician needs more information than a plain x-ray can provide, he might request a CT scan. This study uses several x-rays taken from different angles and combines them to produce images that are cross-sectional views of body structures.
- Magnetic resonance imaging (MRI): This test uses a strong magnetic field and radio waves to provide detailed views of bone and soft tissues. If your doctor suspects an infection or a growth is contributing to the kyphosis, an MRI might be ordered.
Nerve tests
Your physician may order nerve testing if your kyphosis symptoms include any muscle weakness or numbness caused by the kyphosis. Nerve tests can help to determine how well or fast the nerve impulses are communicating between your spinal cord and the rest of your body. Spinal deformity can be noted through reduced speeds of communication between the spinal cord and the rest of your body.
Lung function test
For patients with severe cases of kyphosis, lung function test is conducted to check whether the deformity interferes with the normal functionalities of the lungs. The test is used to check how the lungs breathe in and out, and how they circulate oxygen in the entire body.
In the case of people who experience kyphosis symptoms in their adulthood, additional tests are done to determine the factors leading to the condition. When it comes to how to fix kyphosis that has developed in adulthood, the tests usually depend on other conditions the patient may be having.
These tests may include a one density scan where a physician uses specialized X-ray to determine the strength of your bones. This test is very helpful in diagnosing the underlying conditions causing weakness of your bones.
Kyphosis: Treatment
There are various Kyphosis treatment methods. Your physician will make recommendations for kyphosis treatment based on several factors including:
- - The age of the patient
- - The patient's overall health status and medical history
- - The severity of the kyphosis
- - The patient's ability to tolerate specific procedures, medications or therapies
- - How the disease is expected to progress
- - The preference or opinion of the patient with regard to kyphosis
The kyphosis treatment goals in children are typical to stop the spinal kyphosis from progressing and to help minimize any deformity. Treatment may include any of the following, or a combination of these treatments:
- Observation and examinations at regular intervals: The child or teen will need to be monitored closely and examined by the doctor at regular intervals. How the curve progresses depends on how mature the child's bones are, or how much the bones grow. The kyphosis treatment will slow down or stop when the child goes through puberty.
- Physical therapy: physical therapy is used for Scheuermann’s disease and lumbar kyphosis treatment. The patient is required to lie flat and a pillow is then placed under their scapula region. This process assists in stretching the cervical spine.
- Bracing: bracing is the common method for kyphosis treatment, especially for children. Sometimes doctors recommend a brace for kyphosis treatment if the child is not finished growing. However, the brace used is determined by the curve pattern. The kind of brace prescribed and the length of time the child will need to wear it varies, and is determined by the physician. This kind of treatment is not recommended for patients above the age of 16 as it doesn’t offer any permanent solution to their condition. A brace tends to make the patient feel restricted and this deters a lot of teenagers suffering from kyphosis from using them. But, modern braces are designed in a manner that allows the patient to engage in a wide variety of physical activities.

- Surgery: If the curve is extreme, measuring 75 degrees or greater on an x-ray, and it is continuing to worsen in spite of bracing, surgery will likely be recommended. This rarely occurs in cases of kyphosis. The goal of surgery for severe and progressive kyphosis is to restore the damaged vertebrae so they are as close to their original height as possible. The procedure is called a kyphoplasty. It generally does not require an incision or stitches, and it may relieve the pain and reduce the deformity caused by kyphosis.
The surgical procedures used for kyphosis treatment include spinal instrumentation and fusion. These kyphosis treatment procedures join and strengthen the spinal part which has been damaged, thus offering permanent stability to the spinal cord. Doctors use medically designed instruments like plates, screws, and rods to hold the patient’s spine straight as it heals.
The bony spinal elements can be joined through an adhesive process known as spinal fusion. Surgeons can either perform the process through the chest cavity or from behind using specialized instrumentation.
Any surgical procedure carries a risk of serious complications. In addition to the risks from anesthesia, other complications may develop from surgery for kyphosis including:
- - Weakness, numbness or tingling due to nerve injury
- - Infection in the surgical site
- - Bleeding from the surgical site
- - An allergic reaction from the chemical dyes used to help visualize the spine during the procedure
- - An increase in pain
- - Leakage of the material used to build up the vertebrae
Prevention
Some types of kyphosis cannot be prevented. For example, if Scheuermann’s disease is discovered and treated early the need for surgery may be reduced, but there is no way to prevent this type of kyphosis from occurring. But, there are other kyphosis treatments for kyphosis caused by our lifestyle.
Maintaining a healthy diet which includes adequate amounts of the vitamins and minerals necessary for bone health, especially vitamin D, can help prevent bone disorders like rickets. Nutritional deficiencies can lead to soft or fragile bones which result in abnormal kyphosis of the spine. Seeking adequate medical care following a traumatic accident or injury, and following the doctor’s instructions can help reduce the risk of post-traumatic kyphosis.
Since many cases of kyphosis in older adults are caused by osteoporosis or thinning bones, preventing or treating osteoporosis can help maintain the spine’s normal curve. Some of the ways to treat osteoporosis are the same methods used to prevent kyphosis from occurring. These kyphosis prevention methods include:
- - Maintaining a healthy body weight
- - Increasing the amount of weight-bearing exercise, such as walking
- - Decreasing the amount of caffeine and alcohol consumed
- - Stopping smoking to prevent osteoporosis and kyphosis.
- - Making sure your intake of calcium and vitamin D is adequate, through diet and supplements.
- - Preventing accidents especially falls in older adults.
- - Consulting your physician about medication, especially if you are a woman who has gone through menopause.
The risk of postural kyphosis can be reduced by becoming more aware of your posture. Encourage your child to develop habits which include:
- - When sitting, avoid slouching the shoulders and back. Maintain an upright position, making sure to provide support for the lower back (the "small" of the back).
- - Choose well-designed backpacks that distribute weight evenly. Avoid heavy book bags that pull on the back and shoulder ligaments and muscles.
- - Regular exercise can help keep the back flexible and strengthen the muscles. Walking, running or swimming are excellent activities to prevent back problems and kyphosis from occurring. Additionally, other exercises like yoga and pilates are extremely beneficial to kyphosis patients. They are ideal for the joints as they stimulate bone redevelopment. Water aerobics are recommended for patients struggling with deteriorating bone diseases like osteoporosis.
- - Standing posture – this can easily be overlooked but can affect your spine’s health in the long-term. It’s good practice to always ensure that the shoulders and back are aligned when standing. You can also engage the stomach muscles to assist in proper alignment. If your profession requires you to bend over regularly, it is advisable to use ergonomic aids.
- - Holding a smartphone or tablet – did you know that the way we hold our phones or tablets has a long-term effect on our spine and, if done right, can play an important role in kyphosis prevention? For the most part, we use these devices when in a hunched position. This habit leads to stiffness and long-term damage to the spine. Therefore, always ensure you are in a forward-looking position when using your mobile device.
- - Seated posture at a computer – every doctor agrees that posture is the largest contributor to unnatural bending of the spine. When using a computer, ensure that the monitor’s position is at eye level and your feet are flat on the floor and the keyboard is placed at the same Scheuermann's with your waist.






