Myelopathy

Myelopathy (Ruptured Discs)
Myelopathy is a medical term that is used to describe any neurological disorder of the spinal cord. It is typically caused by compression of the spinal cord due to bone spurs, also known as Osteophytes, or by herniated or “ruptured” discs in the cervical spine. The cervical vertebrae are located in the neck area of the spine. Ruptured discs can occur in many different medical disorders which cause neck pain. Some of these conditions are:
- Central Cord Syndrome
- Partial Brown-Sequard Syndrome
- Motor System Syndrome
- Transverse Syndrome
- Mixed Radicular and Long Tract Syndrome
- Myelopathy pain may be due to abnormalities in the bones of the spine (vertebrae) and facet joints (joints that work together and allow you to bend and turn your neck), or it may be caused by problems in the nerves, muscles, and ligaments of your spine
Myopathy is a different condition and not to be mistaken for Myelopathy, which has to do with nerve damage inside the spinal cord. Myelopathy and ruptured discs may occasionally be in conjunction with Radiculopathy. Radiculopathy is the term used to depict squeezing of the nerve roots as they leave the spinal cord or cross the intervertebral disc, instead of the pressure of the line itself (Myelopathy).
Myelopathy can happen in any region of the spine and has an alternate name contingent upon where in the spine it shows up.
Cervical Myelopathy
Cervical Myelopathy happens in the neck and is the most widely recognized type of Myelopathy. Neck pain is one of the side effects of Cervical Myelopathy, however, not all patients encounter it.
Thoracic Myelopathy
Thoracic Myelopathy happens in the central region of the spine. The spinal cord in this region gets compressed because of swelling or ruptured discs, bone spurs, or spinal injury.
Lumbar Myelopathy
Lumbar Myelopathy is an uncommon condition in light of the fact that in the vast majority, the spinal cord closes in on a segment of the lumbar spine. If the spinal cord is low-lying or fastened, it can be influenced by Lumbar Myelopathy.
Prevalence
Myelopathy is also known as spinal cord compression. It is one of the most common reasons for cervical (neck) pain in people living in the United States who are older than 55. Many people with spinal stenosis have symptoms such as numbness, weakness, burning, pain and tingling sensations. Up to 10% of these people may also develop Myelopathy.
Causes of Ruptured Discs
One of the most common causes of Myelopathy is everyday wearing and tear. In fact, Myelopathy is one of the most frequent reasons people who are aging develop neck pain. As the body grows older, stress caused by everyday wear and tear brings about degenerative changes. The changes that occur affect the discs between your vertebrae, your ligaments and your facet joints and these changes can cause Myelopathy.
As you grow older, the discs between your vertebrae start to dry out and harden. This causes them to shrink, and the space between the joints that allow you to move freely starts to close. This adds stress to the cartilage that keeps the vertebrae functioning. More degeneration starts to occur because of this added stress.
As the vertebral discs degenerate, they can also herniate or rupture. This can add additional pressure to your spinal column by pressing on your nerve roots or on the spinal cord. Bone spurs also form as a result of degeneration and wear and tear. Bone spurs can take up space in the spinal canal, making it narrow and compressing or pinching the spinal cord and causing Myelopathy.
Accidents and injuries also commonly contribute to myelopathy. Injuries sustained in sporting or motor vehicle accidents or in falls often affect the stabilizing ligaments and muscles of the spine. Injuries can also cause dislocations of joints and bone fractures which contribute to Myelopathy. Central Cord Syndrome is also frequently the result of an injury.
Another cause of Myelopathy can be an inflammatory disease process such as Rheumatoid Arthritis. This disorder attacks the joints of the spine and typically affects the upper neck area.
Other causes of Myelopathy that are less common include infections, tumors, and abnormalities of the spinal column which are present at the time of birth.
As you age, aggravation, ligament ailment, bone spurs and the straightening of the spinal discs between the vertebrae can put weight on the spinal cord and the nerve roots. Myelopathy regularly grows gradually as after effect of the progressive degeneration of the spine (spondylosis), yet it can likewise take an intense shape or originate from a spine distortion display during childbirth.
- Normal reasons for Myelopathy are degenerative spinal conditions, for example, spinal stenosis, a narrowing of the hard ways of the spine through which the spinal line and nerve roots travel.
- Focal disc herniations can likewise bring about pressure on the spinal cord, prompting the advancement of Myelopathy.
- Immune system issues, for example, rheumatoid joint pain in the spine, can likewise prompt degenerative changes in the vertebrae that get damaged in spinal cord pressure and Myelopathy.
- Hernias, growths, hematomas and spinal tumors, including bone malignancy, may likewise push on the spinal cord and prompt Myelopathy.
- Intense Myelopathy can grow rapidly because of spinal damage, spinal contamination, provocative ailment, radiation treatment or neurological issue.

At the point where the spinal cord is compacted or harmed, it may cause a loss of sensation, loss of movement, and pain or uneasiness in the area at or beneath the pressure point.
The correct indications will rely upon where in the spine Myelopathy is present. For instance, Cervical Myelopathy is probably going to have side effects in the neck and arms.
Most often the Myelopathy symptoms include stiffness in the neck, a deep and aching pain on one or both sides of the neck and pain in one or both of the arms and the shoulders. Weakness and stiffness in the legs and difficulty walking can also be Myelopathy symptoms. Some people experience a grinding, crackling or grating sensation when they move their neck.
Other common myelopathy symptoms include:
- Stabbing pains in the upper extremities: upper arms or elbows, or the wrist and fingers
- Dull and aching sensation in the arm, or a loss of sensation; numbness is also a common symptom of Myelopathy
- A sensation called “position sensory loss.” This is being unable to sense where your arms are unless you can see them
- Loss of bladder control can be a sign of severe Myelopathy
These Myelopathy symptoms usually come on gradually, over the course of several years. Many times the signs of Myelopathy may not be noticed until the spinal cord has been significantly compressed, by at least 30%.
Diagnostic procedures
In order to diagnosis Myelopathy, many physicians start by obtaining a medical history and completing a thorough physical examination. Doctors who suspect Myelopathy will pay special attention to the patient’s reflexes, looking for an over-active or exaggerated reflex, which is known as hyperreflexia. Doctors who suspect Myelopathy will also often look for weakness in the muscles of the upper arms, and atrophy, which is a deterioration and shrinkage in the size of the muscles. They will also assess for numbness or loss of feeling in the arms and hands.
If your physician suspects you may have Myelopathy, based on the results of your medical history and his physical assessment, he may order additional tests.
Manifestations of Myelopathy are not uniform in this condition. Your specialist may prescribe the accompanying tests to limit the Myelopathy conclusion:
- An x-ray to discover different issues
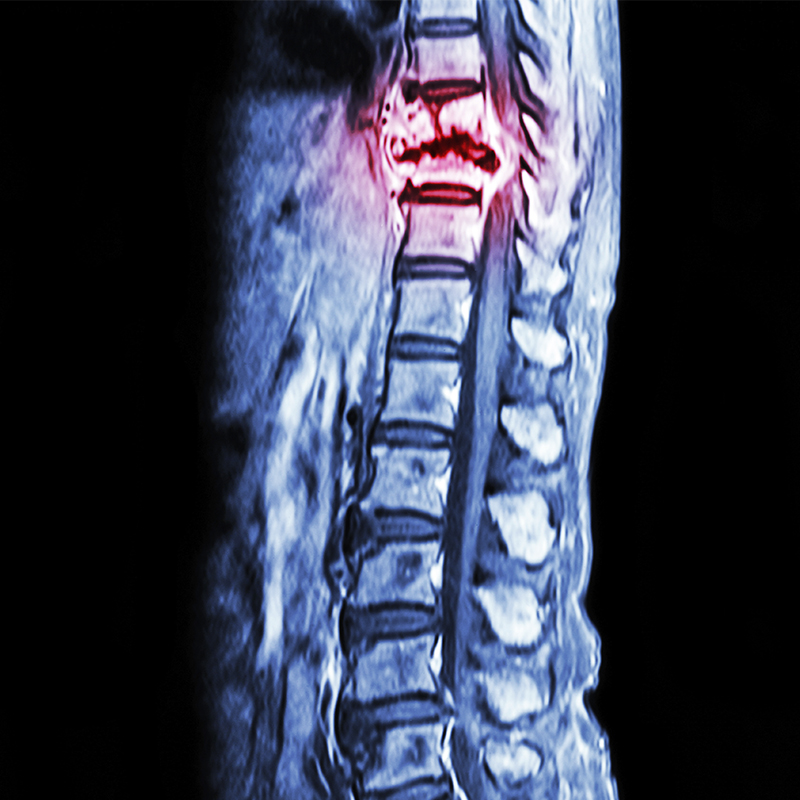
- An MRI check for an in-depth look at the spine and spinal column, which can indicate zones of stenosis
- Myelography utilizes a differentiation material and a constant type of an X-ray called fluoroscopy to uncover variations from the norm of the spinal line. It is some of the time utilized rather than MRI for patients who can't be inside an MRI machine.
- Electrical tests, for example, an electromyogram or somatosensory evoked possibilities, indicate how well your nerves are working to give sensation and development capacity to your arms and legs. These tests measure how nerve incitement in a hand, arm, leg or foot is transmitting through the spinal cord to the brain.
The finding itself might be imparted to you by your specialist in a few distinctive ways. Some of the time, Myelopathy is included toward the finish of another basic condition to demonstrate the inclusion of the spinal cord. For instance, your specialist may disclose to you that you have Cervical Stenosis with Myelopathy or a Thoracic Disc issue with Myelopathy.
In the event that Myelopathy is a difficulty of another illness, your specialist may allude to it in the terms of this infection. For instance, Diabetic Myelopathy implies that the spinal cord has been harmed because of diabetes. Carcinomatous Myelopathy implies that the spinal cord has endured harm because of a carcinoma.
Myelopathy Treatment
Myelopathy treatment relies upon the reasons for Myelopathy. In any case, now and again, the reason might be irreversible, so the treatment may just go the extent that helping you calm the side effects.
Nonsurgical Myelopathy Treatment
Nonsurgical treatment for Myelopathy may incorporate propping, exercise-based recuperation and similar options. These treatments can be utilized for mild Myelopathy and are good for decreasing pain and helping you get back to your day to day activities.
Nonsurgical treatment that does not eradicate the pressure may advance the side effects — normally slowly, however in some cases intensely, in a few occurrences. On the off chance that you see the movement of your side effects, converse with your specialist as quickly as time permits. A portion of the movement can be irreversible even with treatment, which is the reason it's critical to stop any movement when distinguished in the gentle stages.
Surgical Myelopathy Treatment
Spinal decompression surgery is a typical Myelopathy treatment to soothe pressure on the spinal column. A surgery can likewise be utilized to extract bone spurs or ruptured discs if that they are determined to be the reason for Myelopathy.
For extreme Myelopathy caused by stenosis, your specialist may prescribe a surgical system to build the channel space of your spinal cord (Laminoplasty). This is a movement saving technique, which implies your spinal cord holds adaptability at the site of the pressure. For different reasons, a few patients may not be suitable for a Laminoplasty. An option is decompression and spinal combination that should be possible anteriorly (from the front) or posteriorly (from the back). Amid spinal combination, vertebrae are intertwined to increase movement in the affected section of the spine.
Non-obtrusive spine surgery may offer alleviation with a lower chance for difficulties and a possibly speedier recuperation than regular open surgery methodology.
While you're anticipating surgery, a mix of activity, way of life changes, ice and heat compressions, infusions, or oral pharmaceutical can enable you to control any painful side effects. It's essential to take any prescriptions precisely as your physician prescribes them since many pain drugs and muscle relaxers can cause reactions, particularly when taken for extended periods of time.
Conservative Myelopathy Treatment
Surgical decompression of the spinal cord is often recommended as the best form of treatment for many patients with Myelopathy. However, in cases where the patient’s symptoms are mild, watchful waiting can be an appropriate approach.
If your symptoms of Myelopathy are mild, your physician may recommend you wear a brace. This will help support and immobilize your cervical spine. He may also suggest exercises to help improve the strength and flexibility of your neck. Pain medications are also often recommended, such as nonsteroidal anti-inflammatory drugs (NSAIDs) for Myelopathy.
Some authorities advise against treating Myelopathy with a conservative approach as conservative methods have not been shown to be beneficial, and in some cases have caused neurological complications.
Epidural steroid injection (ESI)
Epidural injections are sometimes used to control the pain of muscle sprains or strains that cause Myelopathy. They also decrease swelling and inflammation. Steroid injections consist of a combination of an anti-inflammatory steroid known as cortisone, and an anesthetic to numb the site of the injection. The medications are given directly to the site of inflammation through the skin, into the epidural space. ESI is not always successful in relieving the symptoms of Myelopathy and is used only if other treatments have been unsuccessful.

Surgical Treatment
The primary goal of surgical procedures for Myelopathy is to take pressure off the spine. One common procedure, a Laminotomy, is completed through an incision made in the back. This opens the spinal vertebrae to give the spinal cord more room. There are risks associated with this procedure for treating Myelopathy, and it may not be appropriate for some patients. It can lead to complications such as the development of Kyphosis, which is an abnormal curving of the spine, causing it to bulge outward at the upper portion, and it could also cause areas of the spine to become unstable. The surgeon may also choose to use an anterior cervical approach to treat Myelopathy, in which an incision is made in the front of the neck, and any disc materials or bone spurs that are causing pressure on the spinal cord are removed. A spinal fusion may also be performed during the procedure for Myelopathy to lessen the risk of postoperative complications.
Myelopathy and spinal column wounds can be complex medicinal issues. At times, pressure or weight on the spinal column will put pressure on nerves. This may cause pain, muscle weakness, or an absence of control. In the event that you have muscle weakness and pain, it may be recommended that you consider surgery keeping in mind the end goal to calm the weight on the nerves. After extended periods of time, pressure on a nerve can do permanent damage. While numerous cells in the body can repair themselves, nerve cells can be irreversibly damaged.






