Osteomyelitis
Osteomyelitis: Definition
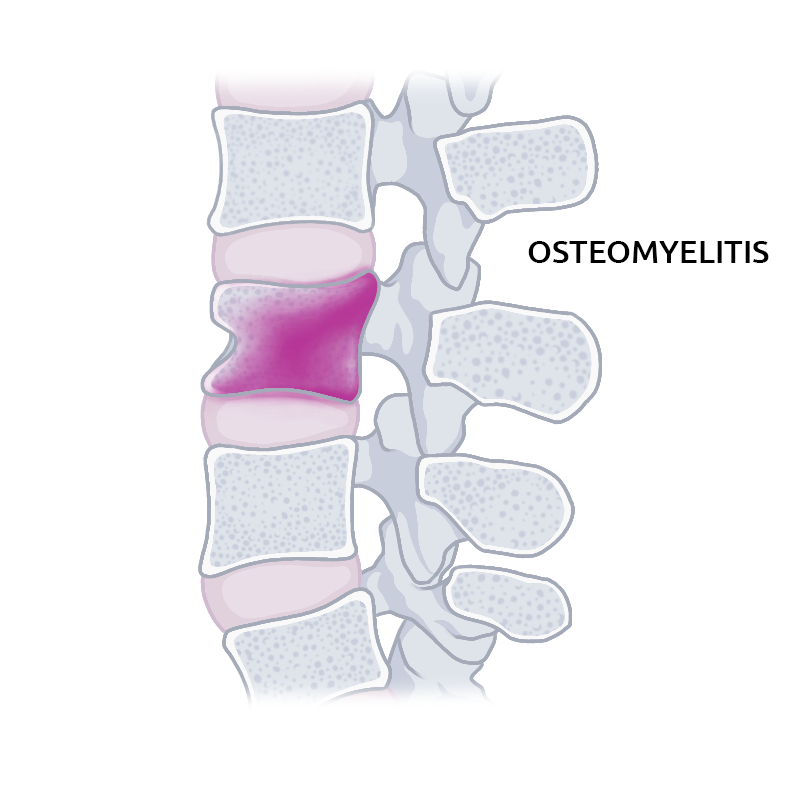
Osteomyelitis is an infection of a bone. The condition can occur in people of any age, but it is more likely to happen in the elderly or in young children. Most of the time Osteomyelitis is a bacterial or a fungal infection. It is typically found in the vertebrae, the bones of the spine, but it is able to spread to the discs that lie between the vertebrae and into the space that surrounds the spinal cord. Osteomyelitis can also occur in bones that have been damaged, injured or have undergone surgical procedures, or in the bones of diabetic's feet.
Prevalence
Approximately one out of every 675 admissions to the hospital every year in the United States is because of Osteomyelitis. That translates to about 50,000 cases annually. Some research indicates that almost half these cases (47%) are considered to be post-traumatic Osteomyelitis. Another main cause of the condition is an infection that is carried in the bloodstream. This is known as Haematogenous Osteomyelitis and it occurs mainly in children. 85% of the cases of this type of bone infection occurs in children who are less than 17 years old. Osteomyelitis can also be caused by neuropathy, and this mostly occurs in individuals who have diabetes. Neuropathy is an abnormality or disorder of the nervous system.
Risk factors
Under usual circumstances, the bones are resistant to infection. In order for Osteomyelitis to develop, a condition that causes your bones to become vulnerable must be occurring. Some of these conditions include:
- Recent orthopedic surgery or a recent injury: Injuries like deep puncture wounds or animal bites give germs a place to enter a bone or tissues nearby and cause osteomyelitis. Severe broken bones or operations to repair these breaks or to replace joints can also open a path for infection.
- Disorders of the circulatory system: The body can't circulate its cells that fight infection when the blood vessels are blocked or damaged. Without these cells, a small infection can grow larger and deeper. What started as a small scratch or blister can grow into a deep wound. This exposes deep tissues and bone to bacteria or other germs that cause serious infection and osteomyelitis. Conditions and diseases that cause impaired circulation include diabetes, peripheral arterial disease, which is often due to smoking, and sickle cell disease.
- Conditions that require treatment with intravenous lines or catheters: Many diseases and conditions require treatment with medications and other fluids administered through the blood vessels. Catheters or tubes are used to remove fluids from your body. The medical catheter or tube used in these procedures increases your risk of a generalized infection that can lead to Osteomyelitis. This is because they serve as a vehicle for transporting germs into your body. Some examples of circumstances when the medical tubing is used in this way include:
- Intravenous tubing and central line tubing
- Urinary bladder catheters
- Kidney dialysis tubing
- Conditions or diseases that weaken the immune system: The immune system can be suppressed by medications or by medical conditions, and this increases the risk for Osteomyelitis. For example, the immune system can be weakened by:
- Chemotherapy medications increase the risk for osteomyelitis
- Diabetes that is poorly controlled increases the risk for osteomyelitis
-
- Anti-rejection medications following an organ transplant
- Corticosteroid medication use increases the risk for osteomyelitis
- Medications called tumor necrosis factor (TNF) inhibitors
- Illicit drug use: People who inject illegal drugs typically use needles that are not sterile and many don't follow the recommended infection control precautions when giving injections. This places them at increased risk for developing Osteomyelitis.
Reasons
Osteomyelitis is an infection of the bone. The most common germ found to cause all types of Osteomyelitis is Staphylococcus aureus. (S. aureus). The bones most often affected in children are the long bones and in adults, the pelvis and the vertebrae are most often affected.
Acute Osteomyelitis: This occurs almost exclusively in children. Adults who develop this form of the condition often have compromised immunity due to IV drug abuse, overall poor health, infectious teeth that have been treated with root-canals, are on immunosuppressive drug therapy or because of other medications or diseases.
Tubercular Osteomyelitis: This occurs as a complication in up to 3% of patients who have pulmonary tuberculosis. The bacteria spread through the patient's circulatory system to the bone, first affecting the joint tissues and then moving into the bone. The vertebrae and the long bones are most often affected in this form of Osteomyelitis. This form of Osteomyelitis affecting the spine is sometimes called Pott's disease.
Haematological osteomyelitis: This Osteomyelitis is carried through the bloodstream and is most often seen in children. Most cases are caused by S. aureus. In infants, it is most commonly caused by Group B streptococci but is also often caused by S. aureus and Escherichia coli (E. coli.) When IV drug users and patients who have had their spleen removed develop this form of osteomyelitis, the cause is frequently Gram-negative bacteria, including bacteria that normally live in the intestines.
Post-Traumatic osteomyelitis: This is the form of Osteomyelitis most common in adults. It is caused by trauma that exposes the bone to infection. S. aureus is the most common bacteria in this case, but other organisms are also common such as E. coli, Serratia marcescens, and Pseudomonas aeruginosa. Most cases of post-traumatic Osteomyelitis have more than one organism contributing to the infection.
Fungal infections that are present in the body can also spread to the bone and cause Osteomyelitis. The most common is Coccidioides Immitis and Blastomyces Dermatitidis.
About 50% of the cases of Osteomyelitis of the spine are due to Staphylococcus aureus and the other 50% are due to tuberculosis infection spread from the lungs to the vertebrae.
Classification
The definition of Osteomyelitis is broad and it takes in a variety of different conditions. According to traditional methods, the duration of the infection, whether the bone has increased in density and whether pus has formed are used to classify the disease.
Chronic Osteomyelitis is often defined as Osteomyelitis that has been present for longer than one month. Some believe there are no well-defined sub-types, but there is a wide variety of characteristics related to the condition that can help define the severity and type of Osteomyelitis.
Osteomyelitis can also be classified according to which bone it affects. For instance, Osteomyelitis in a large bone is different in many ways from Osteomyelitis in the jaw or in the vertebrae.
Osteomyelitis Symptoms
Osteomyelitis symptoms can change extraordinarily. In young children, Osteomyelitis symptoms frequently happen all the more rapidly. They create pain or sensitivity over the influenced bone, and they may experience issues or weakness to utilize the influenced bone or to hold up underweight or walk because of extreme pain. They may likewise have fever, chills, and redness at the site of contamination.
In adults, the Osteomyelitis symptoms frequently grow more steadily and incorporate fever, chills, dizziness, swelling or redness over the influenced bone, tightness, and sickness. In individuals with diabetes, peripheral neuropathy, or peripheral vascular ailment, there might be no fever or pain. The main Osteomyelitis might be a zone of skin breakdown that is intensifying or not recuperating.
Osteomyelitis symptoms may often include:
- Fever and perspiration or sweating
- Generalized weakness
- Severe, ongoing back pain that increases with movement
- Unexplained weight loss
- Redness, warmth, swelling, and tenderness at the site of infection
If Osteomyelitis is located in the vertebrae, the patient may experience muscle spasms or pain in the back without a fever. If the infection involves the spaces surrounding the spinal cord, severe back pain that radiates to other sites, such as down the legs or into the neck or arms may occur, as well as weakness in the muscles and paralysis.
Sometimes Osteomyelitis symptoms cannot be cured completely. It may then turn into a less severe form of Osteomyelitis that comes and goes intermittently for several months or even years. This is called Chronic Osteomyelitis. Osteomyelitis symptoms may include bone pain and tenderness and sinus drainage. Infections in the bones can block blood supply and lead to the death of parts of the bone. This causes Osteomyelitis symptoms to spread and abscesses may form that drain through the skin.
Diagnostic Procedures for Osteomyelitis Symptoms
If your doctor suspects you have Osteomyelitis symptoms, he may order procedures and tests to confirm the diagnosis and to determine what organism is causing the infection in the bone.
Your specialist may utilize a few strategies to analyze your condition in the event that you have any side effects of a bone disease. They will play out a physical exam to check for swelling, torment, and staining. Your specialist may arrange lab and indicative tests to decide the correct area and degree of the contamination.
It's imaginable your specialist will arrange a blood test to check for the creatures causing the contamination. Different tests to check for the microscopic organisms are throat swabs, urine tests, and stool examinations.
Another conceivable test is a bone culture, which uncovers the cell and metabolic action in your bones. It utilizes a radioactive substance to feature the bone tissue. In the event that the bone scan doesn't give enough data, you may require an MRI check. Now and again, a bone biopsy might be fundamental.
In any case, a straightforward bone X-ray might be sufficient for your specialist to decide the treatment.
Blood tests
Blood tests can show if your white blood cells are elevated, and may also reveal other factors to indicate an infection is present in your body. If the Osteomyelitis symptom was caused by an organism in your bloodstream, blood tests might show what germs are responsible and what medications can effectively fight against them. There is no blood test to determine whether you have osteomyelitis symptoms, but your blood work does help your physician know what further procedures or tests you might need.
Imaging tests
- X-rays: Damage to your bones will be visible on X-rays, but the damage caused by Osteomyelitis may not be detected on an X-ray film until it has been in your bone for several weeks. If your Osteomyelitis symptoms are more recent, you may need tests that can provide more detailed images.
- Computerized Tomography (CT) scan: This test uses X-rays taken from several different angles and combines them to create very detailed cross-sectional images of your internal structures. Damage caused to your bones by Osteomyelitis will appear much sooner on a CT scan than on a standard X-ray.
- Magnetic Resonance Imaging (MRI): This test uses strong magnets and radio waves to produce images of bones and soft tissues that are very detailed. Your doctor may order an MRI if he wants to view the details of tissues surrounding your bones that might be affected by Osteomyelitis.
Bone biopsy
A bone biopsy is a procedure most commonly used for diagnosing Osteomyelitis symptoms. It can confirm the presence of infection in the bone and it can also reveal what organism is responsible for the infection. When your doctor knows what organism is present, he can choose the antibiotic that will work best to treat that particular infection.
An open bone biopsy is a surgical procedure and requires anesthesia. In other cases, the surgeon uses a long needle inserted through your skin into the affected bone to obtain a specimen. In this case, medication is given to numb the area prior to insertion of the needle, and imaging scans or X-rays are sometimes used to guide the placement of the needle.
Treatment for Osteomyelitis
Most of the time, Osteomyelitis can be treated with anti-toxins and pain drugs. In the event that a biopsy is used, this can help manage the decision of the best anti-infection. The term of treatment for Osteomyelitis with anti-infection agents is normally four days to two months, however, it differs with the kind of contamination and the reaction to the medications. Now and again, the influenced area will be immobilized with a support or brace to diminish the agony and speed the process of treatment for Osteomyelitis.
Treating Osteomyelitis usually involves hospitalization. Most commonly, antibiotics are used to treat the infection, and occasionally surgery is needed to remove parts of bone that are dead or infected.
Once in a while bone diseases require surgery. On the off chance that you have surgery, your specialist will extract the infected bone and dead tissue and deplete any abscesses, or pockets of discharge.
On the off chance that you have a prosthesis that is causing the disease, your specialist may replace it with another one. Your specialist will likewise extract any dead tissue close or be encompassing the tainted region.
Medications
A biopsy of the infected bone will show what kind of organism or germ is causing the infection. This information will enable the doctor to use an antibiotic that works well to eliminate that specific kind of infection. The most common way for the antibiotics to be administered initially for Osteomyelitis is through a vein. Treatment for Osteomyelitis usually lasts from 4 to 6 weeks. Some antibiotics cause side effects like diarrhea, upset stomach and vomiting. After the course of intravenous antibiotics, the treatment for Osteomyelitis is completed, and as additional, taken by mouth may be necessary for infections that are more severe.
Surgery
Depending on how severe the infection is, treatment for Osteomyelitis may include one, or a combination of the following surgical procedures:
- Drainage of the area that is infected: This involves making an incision in the area surrounding the affected bone. The surgeon is then able to drain any fluid or pus that has accumulated due to the infection.
- Debridement of the diseased tissue and bone: In a procedure called surgical debridement, the surgeon cuts away as much of the infected bone as possible and removes a small portion of healthy bone as well. This is to make sure that all the diseased portions have been there. If surrounding tissues show any signs of disease or infection with osteomyelitis, they may also be removed.
- Repair of blood vessels: Empty space may be left by the debridement, and the surgeon may fill this space with a portion of healthy bone or tissue like skin or muscle from another a procedure of the body. Temporary fillers are used sometimes to fill the space until the patient is well enough to tolerate a bone or tissue graft. The graft aids the body in forming new bone and repairing blood vessels that have been damaged by osteomyelitis.
- Removal of foreign objects: Sometimes foreign objects or materials such as surgical screws or plates, which were inserted during a previous surgical procedure need to be removed.
- Amputation: The affected limb may have to be surgically amputated as a last resort, in order to stop the spread of osteomyelitis.
Hyperbaric oxygen therapy
In cases of Osteomyelitis that are very difficult to treat, hyperbaric oxygen therapy can help deliver more oxygen to the infected bone, which promotes healing. Hyperbaric oxygen therapy is carried out using a chamber that is pressurized and looks like a large cylinder.
Prevention
The best way to prevent Osteomyelitis from occurring is by trying to avoid infection in general, especially if have a weakened immune system. Keep things clean and avoid getting cuts or scrapes. If you or your child to get a scrape or a cut, clean the area right away and bandage it using a clean bandage. Check the area often and report any signs of infection to your doctor: redness, swelling, warmth, discolored drainage or odor or increased pain in the area.
If you have a history of Osteomyelitis or you have chronic osteomyelitis, be sure your doctor has your complete medical history. This way, you can work with your doctor on a plan for prevention and for treatment for Osteomyelitis that is right for you. If you are a diabetic, be sure to inspect your feet daily and notify your doctor if you notice any changes. The sooner Osteomyelitis is diagnosed and treated, the better your chance of recovery.
If acute Osteomyelitis is detected and treated early, it can be prevented from becoming a chronic illness that requires ongoing monitoring and medication. Early detection and prompt treatment for Osteomyelitis not only relieves the pain and the need for medical care due to repeated infections, it improves the chances of recovery.






