Spinal Stenosis
Spinal Stenosis: Definition
What Is Spinal Stenosis?
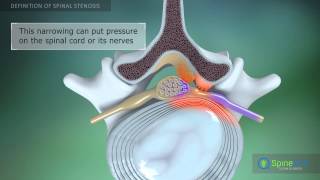
Spinal stenosis is a condition that occurs when the spaces in your backbone (spine) become narrow. When this happens, your spinal cord and its nerves can become compressed or pinched. More than half the time, spinal stenosis occurs in the lumbar spine, which is the lower portion of the back, and the narrowing of the spine that goes along with this condition causes pain that travels down the back of the leg.
In general, there are 3 major classifications of spinal stenosis.
- Foraminal spinal stenosis is the most common type of lumbar spinal stenosis, may also be referred to as lateral spinal stenosis. As the nerve root is about to leave the canal through a side hole at the back of the spine, called the neuro-foramen, a bone spur (osteophyte) that has already developed from bone degeneration or arthritis, can press on that nerve root.
- Central spinal stenosis occurs when the central spinal canal is constricted with enlarged ligament and bony overgrowth, causing compression of the spinal cord and cauda. This narrowing can cause pressure on the nerve bundle at the end of the spinal cord (cauda equina) or the nerve bundle within the thecal sac. Stenosis can occur along any area of the spines, but most common in the lumbar area
- Far lateral spinal stenosis is the narrowing of the area lateral, or to the side of the neuro-foramen. The narrowing is secondary to the development of bone spurs from the facet joints, bulging discs, herniated discs, and ligament hypertrophy.
Spinal Stenosis Causes
Reasons Why Spinal Stenosis Happens
Some people are born with an unusually small spinal canal. In other cases, spinal stenosis comes about when another condition or disorder occurs that reduces the amount of space in the canal.
Spinal stenosis may be caused by:
- Bone Spurs: Bone spurs are one of the common spinal stenosis causes. They form when wear and tear damage causes extra bone tissue to form. If these develop in the spinal canal, they can cause spinal stenosis. Paget's disease is a bone disorder that typically occurs in adults that can also cause the overgrowth of bone material.
- Herniated Discs: Spinal stenosis can also be caused by ruptured or herniated intervertebral discs and are common spinal stenosis causes. These are the soft cushions between your vertebrae that serve as shock absorbers. As the body ages, these discs dry out. If the outer rim cracks or tears, some of the soft gel-like material from the inside can leak out, causing spinal stenosis by pressing on the spinal cord and nerves inside the spinal canal.
- Stiff and Thickened Ligaments: Ligaments are tough fibers that help add stability to the spine by binding the vertebrae together. Over time, these ligaments get hard and thicken. As this happens, they can sometimes bulge and decrease the amount of space in the spinal canal, leading to spinal stenosis.
- Tumors: Abnormal tissues or masses sometimes grow inside the membranes of the spinal cord, or in the space between the spinal cord and the vertebrae, taking up room in the spinal canal. This causes spinal stenosis.
- Injuries or Trauma: Falls, motor vehicle accidents or other injuries and trauma can cause serious dislocations or fractures of one or more backbones. These fractures or dislocations can be one of the common spinal stenosis caused by damaging the spinal canal. Sometimes surgery on the spine can cause swelling in tissues near the spinal canal that compress the spinal nerves and the spinal cord.
- Malignancy or cancer is abnormal growth of the spinal cord or within the membranes covering the cord and the vertebrae. It's one of the rare spinal stenosis causes
- Spinal ligament changes such as inflammation and scarring can result in thickened ligaments. These thickened ligaments can impinge the spinal canal over time.
- Spinal cord abscess is a collection of pus from an infection. This swollen area can cause permanent damage to the spinal cord
- Spondylolisthesis is a condition when a vertebra slides forward on the vertebra below it, commonly seen in the lumbar spine.
Prevalence
Who Is At Risk?
Spinal stenosis occurs most often in people who are older than 50 years of age. People who develop the condition at a younger age most often have a genetic disease that has affected the development of their bones and muscles.
Risk Factors
The main risk factor for spinal stenosis is the age over 50 years. Other predisposing factors are the following:
- Genetically abnormal narrowing of the spinal canal
- Developmental problems in the spine prior to birth
- Poor posture and body mechanics
- Degenerative disc disease
- Obesity
- Smoking
- Diseases such as arthritis, scoliosis, osteoporosis, and lordosis.
Complications

Spinal Stenosis: Symptoms and Diagnostic Procedures
What Are the Symptoms of Spinal Stenosis?
The primary clinical symptoms of spinal stenosis are chronic pain. In patients with severe stenosis, weakness and regional anesthesia may result. Patients with spinal stenosis become symptomatic when pain, motor weakness, paresthesia, or another neurologic compromise causes distress. Spinal stenosis of the thoracic spine is more likely to directly affect the spinal cord because of the relatively narrow thoracic spinal canal.
Spinal stenosis of the cervical and thoracic regions may contribute to neurologic injuries, such as the development of a central spinal cord syndrome following spinal trauma. Spinal stenosis of the lumbar spine is associated most commonly with midline back pain and radiculopathy. In cases of severe lumbar stenosis, innervation of the urinary bladder and the rectum may be affected, but lumbar stenosis most often results in back pain with lower extremity weakness and numbness along the distribution of nerve roots of the lumbar plexus.
Spinal canal size is not always predictive of clinical symptoms of spinal stenosis, and some evidence suggests that body mass may play a role in limitations of function in this population. Severe radiologic stenosis in otherwise asymptomatic individuals suggests inflammation, not just mechanical nerve root compression. Specific inflammation generators may include herniated nucleus pulposus (HNP), ligamentum, flavum, and facet joint capsule.
Sometimes, people who have spinal stenosis have no symptoms of the condition. When symptoms do start to appear, they usually come on gradually and slowly get more severe. The symptoms of spinal stenosis vary and depend on what part of the spine is affected. Evidence of spinal stenosis is usually apparent on X-ray.
- Symptoms in the Neck: If spinal stenosis is present in the neck (cervical area of the spine), it can cause pain and possibly tingling or numbness in the arms or the legs. If it is very severe, incontinence of bowel and/or bladder may result due to compression of the nerves that control these functions.
- Symptoms in the Lower Back: If spinal stenosis leads to nerve compression in the lumbar area (lower spine), symptoms of spinal stenosis might be muscle spasms and cramping and leg pain with standing and walking. The pain is relieved by bending forward or sitting because this removes the pressure from the pinched nerves.
- Leg or buttocks pain and cramping which gets worse on walking, standing straight or leaning backward
- Stiffness in the leg and thighs
- Low back pain
- Loss of bladder and bowel control in severe cases
When Should I See a Doctor?
If you have pain that lasts more than a few days, or if you have numbness or weakness in your legs or arms, or bowel or bladder incontinence, notify your physician. These could be signs of spinal stenosis or a more serious medical condition.
Diagnostic Procedures
How is Spinal Stenosis Diagnosed?
Since the symptoms of spinal stenosis mimic those of many other conditions common to aging, it is not always easy to diagnose. In order to diagnose the particular cause of your pain and other symptoms of spinal stenosis, your doctor may recommend several imaging tests. Recommended tests for spinal stenosis may include:
X-rays: Standard X-ray films usually don't provide doctors with enough information to give a definitive diagnosis of the symptoms of spinal stenosis, but they do help to rule out other reasons for your symptoms.
Magnetic Resonance Imaging (MRI): An MRI uses a strong magnetic field and radio waves to obtain images that a doctor can use to evaluate the condition of your spine and also the soft tissues of the body to locate the area where physical symptoms of spinal stenosis are occurring. An MRI provides much more information than an X-ray and many physicians recommend this test if they suspect spinal stenosis.
CT Myelogram: A Computerized Tomography (CT) uses X-rays taken from many angles and combines them to provide images that are very detailed. A myelogram involves the injection of dye which helps certain structures to appear even more clearly. This is very useful in cases of suspected spinal stenosis because it can show the spinal canal's size and shape, and can reveal bone spurs, herniated discs, and abnormal growths and masses.
Spinal Stenosis Treatment Options
How Is Spinal Stenosis Treated?
These diagnostic studies are usually performed if symptoms do not subside after a period of 3 to 6 months of therapy such as rest, anti-inflammatory medications, and physical therapy.
Neuronal studies include the following:
- Needle electromyography - Can help to diagnose lumbosacral radiculopathy with axonal loss
- Nerve conduction studies - Can help to differentiate lumbar spinal stenosis (LSS) from other confounding neuropathic conditions (eg, lumbosacral plexopathy, generalized peripheral neuropathy, tarsal tunnel syndrome, other mononeuropathies)
- Somatosensory evoked potentials - are useful in the diagnosis of central nervous system (CNS) pathology and are also used intraoperatively during decompressive surgery to assist the physician in dynamically identifying any iatrogenic changes to the sensory pathways
The spinal stenosis treatment options vary, depending on how severe the signs and symptoms are and where in your spine the condition has occurred. Treatment may include:
- Medications: The goal of medications taken for spinal stenosis is to relieve the pain caused by the condition. Several different spinal stenosis treatment options may be recommended by your physician including:
- Non-steroidal anti-inflammatory drugs: These are also known as NSAIDs. They help ease the pain of spinal stenosis by reducing inflammation as well as by decreasing the body's response to pain. Examples are naproxen and ibuprofen. Some NSAIDs can be purchased over-the-counter. Other NSAIDs such as COX-2 inhibitors require a physician's prescription.
- Muscle Relaxants: Muscle relaxants are effective in treating the pain of spinal stenosis because they reduce muscle spasms. Cyclobenzaprine is one example of a muscle relaxant. These medications require a doctor's prescription and one of the common spinal stenosis treatment options.
- Anti-depressants: Some medications that are used to treat depression are also effective for relieving the pain of spinal stenosis. One example is venlafaxine. These medications require a doctor's prescription.
- Anti-seizure drugs: Medications that are used to treat seizure disorders are also useful in controlling pain caused by nerve disorders and can help control the pain caused by spinal stenosis. One example is gabapentin. Again, a physician's order is needed for these types of drugs.
- Opioids: These are narcotic medications. These are usually only prescribed for very severely painful spinal stenosis and they are given for limited amounts of time. An example of a narcotic is oxycodone. A doctor's written prescription is needed to obtain opioids.
- Therapy: Sometimes physical therapy is recommended for patients with one of the spinal stenosis treatment options. A therapist can help with an exercise program that is designed to help:
- Improve the flexibility and stability of the spine
- Improve overall strength
- Improve and maintain balance
- Epidural Injections: Your physician may recommend steroid injections given epidurally for as one of the spinal stenosis treatment options. The goal of these injections is to reduce the swelling and irritation directly in the affected area. Corticosteroids have anti-inflammatory properties and can help ease swelling and reduce the pressure caused by spinal stenosis. Because of the potential side effects of steroids, these injections can only be given a few times per year.
- Surgery: Surgery is not usually recommended unless conservative spinal stenosis treatment options have been unsuccessful or the symptoms of spinal stenosis are so severe they are causing serious disability. The goal of surgery is to decompress or remove the pressure from the spinal cord and nerve roots. A common procedure for spinal stenosis is a laminectomy. In this operation, a part of a vertebra is removed to create more room in the spinal canal. If more stability is needed in the spine, a procedure called spinal fusion may be necessary. In this procedure for spinal stenosis, vertebrae are fused to form one solid piece of bone
Spinal surgery usually helps to ease the symptoms of spinal stenosis, but there are risks associated with any procedure on the spine. These may include:
- Infection
- Blood clots
- Neurological decline or deficit
- Leakage of spinal fluid
- Respiratory problems
- Bleeding
Useful Advice
Useful Home Remedies
There are several things you can do at home to relieve the pain of spinal stenosis:
- Take over-the-counter pain medications to help with inflammation and discomfort
- Try applying cold packs or mild heat to areas that are painful
- Consider using a walker or cane to help relieve the pain of spinal stenosis. These add stability and also allow you to take pressure off your spinal cord and nerves while walking
If your pain is severe, or if you have weakness or numbness in your arms or legs, contact your doctor.






